

Children who experience traumatic experiences have a higher risk of abusing drugs or alcohol as adults. Numerous studies have found a strong correlation between childhood trauma and addiction. For example, in a National Survey of Adolescents, teenagers who experienced sexual or physical abuse were 3 times more likely to report past or current substance abuse than those without a trauma history. Surveys of teens receiving substance abuse treatment also found that 70% of patients had trauma exposure at some point in their lives.
This article will explore the link between childhood trauma and adult addiction. We'll also discuss the psychological mechanisms that might contribute to this connection and provide insights into therapeutic approaches to address these underlying issues.
Childhood trauma refers to experiences during one's formative years that are emotionally or physically harmful and have the potential to disrupt normal development. These experiences often involve a child feeling threatened, frightened, or helpless. Childhood trauma can take various forms, including:
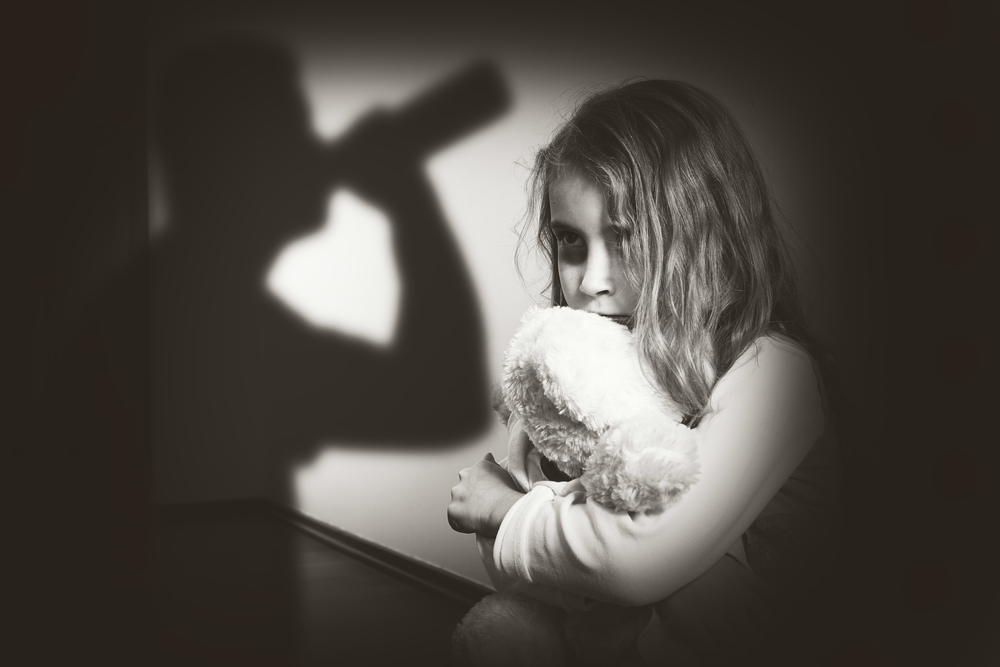
The impact of childhood scars from traumatic experiences can be profound and may manifest in various ways, influencing emotional, cognitive, and behavioral aspects of a person's life. Sadly, about two-thirds of teens and adolescents report experiencing at least one childhood trauma by age 16.
Childhood trauma has been linked to different mental health issues like anxiety, depression, and post-traumatic stress disorder (PTSD). These mental health issues can lead to addiction or exacerbate the symptoms of addiction. Other ramifications include:
Addiction and mental health illness are both chronic brain disorders that often overlap. This means that many people with substance use disorders usually have underlying mental health issues as well.
According to the SAMHSA, about 9 million people have co-occurring disorders. While neither condition leads to the other, they often exist together, and one condition can aggravate the symptoms of the other.
When a child goes through traumatic events during their formative years, it can shape the way their brain develops and processes information. Several interconnected factors contribute to the link between childhood trauma and the development of addictive behaviors.
One such factor is the increased risk of mental health disorders. Childhood trauma increases one’s vulnerability to the development of anxiety, depression, and PTSD. These mental health issues have been found to co-occur with substance use. And the reason behind that is people with untreated mental health diseases are more likely to turn to substances as a form of self-medication.
Traumatic experiences in childhood can overwhelm a child's ability to cope with stress and emotions. In the absence of healthy coping strategies, they may turn to substances as a way to self-soothe, escape emotional pain, or numb distressing feelings associated with the trauma.
Childhood trauma can influence the development of the brain, particularly areas related to stress regulation, emotional processing, and impulse control. These alterations may contribute to a heightened susceptibility to addictive behaviors later in life.
Substance use may serve as a way to escape or suppress painful memories associated with the trauma. Drugs or alcohol can temporarily alleviate emotional distress, providing a perceived sense of relief.

Trauma can negatively impact self-esteem and contribute to a distorted self-perception. Substance use may be employed to help cope with feelings of guilt, shame, or inadequacy resulting from the trauma.
The social and environmental context in which childhood trauma occurs can also contribute to the risk of addiction. Lack of support systems, exposure to substance abuse within the family, or living in environments with high levels of stress and instability can further amplify the risk.
Individuals who have experienced abuse and neglect may be more likely to perpetuate a cycle of trauma within their own families. This intergenerational transmission of trauma can create an ongoing risk for substance abuse across generations.
The good news is that there are different therapeutic approaches to help address underlying issues. Here's a look at some common treatment modalities for teens, adolescents, and adults:
CPT is a type of cognitive-behavioral therapy (CBT) specifically designed to treat PTSD. It aims to help people challenge and modify distorted thoughts and beliefs about the traumatic event. The therapy involves identifying and addressing the impact of trauma on beliefs about safety, trust, power, esteem, and intimacy.
EMDR is a structured therapy that targets traumatic memories and helps one process them. It involves bilateral stimulation, typically through side-to-side eye movements, while the person focuses on distressing memories. This process aims to facilitate the adaptive processing of traumatic information and reduce emotional distress.
NET is an evidence-based therapy designed for those who have experienced multiple or complex traumas. It involves the detailed narration of the individual's life story, including traumatic events. Through retelling the narrative, the therapist helps the person integrate these experiences into a coherent life story, promoting a sense of mastery and understanding.

Play therapy is an approach that utilizes play to help individuals, especially children, express themselves and process their experiences. Therapists can gain insights into the child's thoughts and feelings through various forms of play, such as art, games, or symbolic play. Play therapy provides a non-threatening way for children to communicate and cope with trauma.
In cases where both addiction and mental health issues are present, one will need a comprehensive and integrated approach to treatment. Comprehensive treatment addresses the mental health and substance use issues at the same time as opposed to treating them separately. Co-occurring mental health and addiction treatment usually involves multidisciplinary teams encompassing addiction specialists, health counselors, medical professionals, and social workers who collaborate to provide holistic interventions. Treatment options for co-occurring disorders include:
The integration of various therapeutic modalities ensures a comprehensive strategy that targets addiction and mental health symptoms and promotes overall well-being and resilience.