Addiction is a disease of the brain. It changes how you perceive the world, how you respond to stress, and how you navigate life's challenges. Even in recovery, the neural pathways affected by addiction can continue to influence thoughts, emotions, and behaviors. This is why cultivating mindfulness in recovery from addiction is so crucial.
Mindfulness goes beyond coping; it helps you see the world differently, grow, flourish, and live a more fulfilling life. Many people who practice mindfulness report improved self-esteem, greater enthusiasm for life, and an increased ability to relax. Studies have also established a compelling link between mindfulness meditation and measurable changes in key brain regions associated with memory, learning, and emotion regulation.
Mindfulness is about being fully present and engaged in the here and now rather than getting caught up in worries about the past or future. It involves bringing focused attention to the present moment with an attitude of openness, curiosity, and acceptance. When you practice mindfulness, you pay attention to your thoughts, emotions, bodily sensations, and the surrounding environment.
The essence of mindfulness lies in its non-reactive and non-judgmental stance towards your internal experiences. Instead of getting swept away by your thoughts and emotions, mindfulness encourages you to observe them with a sense of curiosity and compassion. This way, you gain a greater understanding of yourself and the world around you, leading to increased self-awareness, emotional resilience, and overall well-being.

Addiction hijacks the brain's reward system. Substance use triggers the release of dopamine, a neurotransmitter associated with feelings of pleasure and reward, reinforcing the desire to seek out and use substances. Mindfulness meditation has been shown to counteract these effects by modulating activity in the brain's reward circuitry. Studies using neuroimaging techniques have shown that mindfulness practices can:
Specifically, mindfulness meditation has been found to increase gray matter density in the prefrontal cortex, the part of the brain responsible for executive functions such as self-control, decision-making, and impulse regulation. This enhanced prefrontal control over the brain's reward circuitry may help those in recovery exert greater control over cravings and impulses. This makes meditation an essential relapse prevention tool.
People who practice and learn how to apply mindfulness techniques in their recovery journey often experience numerous benefits that contribute to their overall well-being and sustained sobriety. Some of the benefits include:
Addiction leaves behind a trail of regrets, guilt, and shame, trapping you in a cycle of self-blame and rumination. Mindfulness offers a way out of this mental prison by teaching you the art of acceptance and letting go. When you bring awareness to your thoughts and feelings without judgment, you learn to make peace with your past and embrace the present moment with an open heart.

Substance use disorders are caused by dysregulation of neural processes. But, evidence shows that mindfulness can target these neurocognitive mechanisms to produce therapeutic effects on SUDs and promote recovery. Studies also show that mindfulness can improve mental health and help individuals overcome withdrawal symptoms.
The emotional regulation skill empowers you to respond to situations with clarity and composure rather than reacting impulsively or being controlled by your emotions. This can be instrumental, especially for those who abuse pain medication to numb their feelings.
Mindfulness equips you with effective tools for managing difficult emotions, like anger, anxiety and depression, which are common triggers for substance use. Practicing mindfulness allows you to observe the sensations, emotions and thoughts that arise in response to triggers without automatically reacting to them. In doing so, you get to pause and consciously choose how to respond rather than be driven by unconscious impulses. With mindfulness, you can develop greater self-control and resilience against cravings, ultimately supporting your journey towards lasting recovery.
Let's explore a range of mindfulness techniques to use in recovery:
This technique involves sitting still and focusing your attention on your breath, bodily sensations, or a specific object. The goal is to cultivate present-moment awareness and develop a non-judgmental attitude toward your thoughts and feelings. Mindfulness meditation helps enhance emotional regulation, reduce stress, and promote a sense of inner peace. Studies also show that mindfulness meditation reduces pain reports among those with chronic pain and other health conditions.

Deep breathing exercises are simple yet powerful mindfulness techniques. It involves taking slow, deep breaths and paying focus on the sensations of your breath as it moves in and out of your body. This technique can calm your nervous system, reduce anxiety, and promote relaxation. You can practice them anywhere and anytime, which makes them a convenient tool for managing stress and cravings in recovery.
Body scan involves you paying systematic attention to different areas of your body. You can start from the head and move gradually to the toe or vice versa. As you scan through each body part, you observe any sensations, tensions, or discomfort without trying to change them. This technique can reduce stress, promote relaxation, and help you increase body awareness.
As the name suggests, this technique involves walking slowly and deliberately while focusing your attention on the sensations of each step and the movement of your body. As you walk, you can become aware of how your feet make contact with the ground. You also become in tune with the rhythm of your breath, and the sights and sounds around you. Mindful walking can help stay in the moment - it can therefore reduce rumination and promote a sense of calmness.
Mindful eating is when you focus on your eating experience. You smell the aroma of the food, touch its texture and savor the taste as it enters your mouth. When you eat slowly and feel each bite without distraction, you cultivate a greater appreciation for food and become more aligned with your body's hunger and fullness cues. Mindful eating can help prevent overeating, promote healthy eating habits, and deepen your connection to the present moment.
If you, a family member, or loved one is having a hard time implementing mindfulness in recovery or would like more advice on mindfulness strategies, you might benefit from seeing a therapist. A licensed therapist can help you develop personalized mindfulness techniques to match your needs. They can also offer additional support to help you manage cravings and triggers. In the event of a relapse, your therapist may recommend treatment in an inpatient drug rehab – though there are outpatient options, too.
The mind-body connection is like a two-way street between your brain and body. Your emotions, thoughts, and behavior can affect your physical well-being and vice versa. For example, when you are anxious or stressed, you're likely to turn to drugs and alcohol to feel good. But in the long run, substance abuse can cause a spectrum of short- and long-term health issues. That's why mind-body principles are a big part of the addiction treatment and recovery movement. The 12 Steps of AA, NA, CA, etc., feature concepts like letting go, meditation, surrender, and gratitude, all critical components of mind-body medicine.
For years, physical activity has also been seen as a complementary therapy in addiction treatment. Numerous research, with more continuing to emerge, shows exercise, in different forms and intensities, can be a game-changer during addiction recovery. One review of existing literature on exercise and its relationship to substance use found that regular physical activity was linked to lowered use in about 75% of the studies. The review looked at 43 studies with over 3,000 participants and discovered decreased depressive symptoms and improved markers of physical health.
Regular exercise can serve as a healthy alternative to addictive substances. That's because exercise and drugs/alcohol work on the same parts of your brain. They both activate the reward center and trigger the release of feel-good chemicals like serotonin and dopamine. While there's still a need for more research to establish how fitness helps in recovery, studies show it might:
Triggers are situations, places, or emotions that can lead to cravings and relapse. Exercise provides a healthy distraction from these triggers, giving you a different focus and channeling your energy into a positive activity. Engaging in physical activity can also create new routines and patterns that break the cycle of addiction, replacing negative associations with positive ones.
Cravings are intense urges to use a substance, often triggered by stress, boredom, or negative emotions. Exercise can help manage these cravings in several ways. It releases endorphins, natural mood boosters that can counteract the adverse effects of stress and anxiety, reducing the intensity of cravings. Additionally, exercise can be mentally engaging, taking your mind off the craving and allowing it to pass naturally.

Withdrawal symptoms can be challenging, often including fatigue, pain, and insomnia. Physical workout can relieve these symptoms by improving circulation, reducing pain perception, and promoting better sleep. It can also boost mood and energy levels, making it easier to cope with the discomfort of withdrawal.
Sleep disturbances are common in addiction recovery, further impacting mood and stress levels. When done at the right time of day, exercise can significantly improve sleep quality. Regular physical activity regulates circadian system, and makes it easier to fall asleep. Additionally, the calming and stress-reducing effects of exercise can further contribute to better sleep.
Exercise can help you learn, think, focus, problem-solve, and enjoy an emotional balance. It can also improve cognitive function because it increases the flow of blood to the brain, and stimulate the growth of new brain cells. This makes it an effective remedy in addiction recovery since addiction tends to impair cognitive function.

Setting and achieving fitness goals, no matter how small, instills a sense of accomplishment. This positive reinforcement spills over into other areas of life, empowering you to believe in your ability to overcome challenges. The discipline required for regular exercise translates into improved self-control, a valuable asset in maintaining sobriety.
Exercise can be a game-changer in your recovery journey, offering many benefits beyond physical fitness. Here are some workout ideas, routines, and insights to integrate into your daily routine to help you in your recovery journey:
Running, swimming, biking, or dancing are fantastic ways to release endorphins, combat stress, and improve mood. Aim for at least 30 minutes of aerobic exercise or moderate-intensity cardio most days.
Yoga, Pilates, and tai chi combine physical movement with meditation, promoting focus, relaxation, and emotional well-being. These practices can be beneficial for managing cravings and anxiety.
Hiking, biking, or simply spending time outdoors can be incredibly therapeutic. Immersing yourself in nature reduces stress, improves mood, and provides peace and perspective.

From managing mental health disorders to improving brain health, regular physical activity offers a range of benefits. However, there are a few things to take note of to enjoy the many benefits of exercise in recovery:
Remember, working out isn’t just about physical fitness; it's about self-care, empowerment, and building a healthier, happier life. Exercise is an excellent stress reliever – and this makes it an important tool in recovery. Experiment with different activities to find what works for you. And don't hesitate to seek help from a personal trainer, therapist, or addiction recovery specialist. They can provide guidance and support on your journey.
The struggle to overcome addiction and break free from its grasp is an arduous journey, full of challenges and setbacks. And for those who’ve experienced incarceration due to substance-related offenses, this struggle is further compounded by the risk of recidivism. A comprehensive addiction treatment program is a great tool to assist in reducing recidivism.
Recidivism, which is the tendency of individuals to relapse into criminal behavior after being released from incarceration or completing a period of treatment or rehabilitation, poses a significant challenge for those seeking to rebuild their lives.
Research has consistently shown a strong correlation between substance abuse and criminal behavior. According to one study, most people entering the criminal justice system have substance use problems or are using illegal drugs at the time of their arrest. Over 80% of inmates in local jails and state prisons said they had used an illegal drug, and 55% used drugs in the month leading to their arrest.
The sad part is that many of these people commit crimes to get money for drugs. In fact, 16.5% of inmates in state prisons said they committed crimes to get money to buy drugs. Others end up in prison because of the psychopharmacological effects of the substance they abuse. For example, drugs like meth or cocaine increase the chances of engaging in violent crime.

Recidivism is a major problem in the US. A longitudinal study by the DOJ that followed released inmates from 30 states found that:
Going by the numbers, it is evident that addressing recidivism is crucial in breaking the cycle of addiction and criminal behavior. And comprehensive treatment plays a pivotal role in achieving this goal.
Comprehensive treatment combines a range of interventions and support services that targets the physical, psychological, and social aspects of addiction. This holistic approach aims to address the root causes of addiction, promote sustained recovery, and ultimately decrease individuals' likelihood of criminal behavior. Let's explore the various components and therapeutic strategies involved in comprehensive treatment and how they contribute to reducing recidivism rates.
The first component of comprehensive addiction treatment is a thorough evaluation and assessment. This helps identify underlying issues that contribute to one’s use of substances. This includes:
These details allow for a tailored medical care plan that addresses the specific needs of the individual. Evaluation and assessment often happen after stabilization in substance abuse treatment. It can include physical exams and specific tests for diseases or disorders per the patient’s report.
Counseling identifies and addresses the psychological, emotional, and behavioral factors contributing to criminal behavior. It helps individuals develop healthier coping skills and strategies to manage their triggers and emotions. Counseling:
Counseling is essential to substance abuse treatment and often occurs alongside other interventions such as detoxification, inpatient treatment, or outpatient programs.

Comprehensive treatment recognizes that the journey to recovery does not end with completing a treatment program. Aftercare support is crucial for reducing recidivism rates. This support can include aftercare programs, sober living homes, support networks, and ongoing counseling sessions.
Continued guidance and assistance ensure that individuals are better equipped to maintain their sobriety, manage triggers and cravings, and navigate the challenges of everyday life without relapsing. A study found that inmates who joined continuing care after release had reduced recidivism.
Successful reintegration into the community is a significant factor in reducing recidivism rates. Comprehensive treatment includes programs focusing on community integration, such as vocational training, educational opportunities, job placement assistance, and housing support.
These programs help individuals rebuild their lives, establish financial stability, and regain a sense of purpose and belonging, which reduces the likelihood of engaging in criminal activities. According to a meta-analysis of programs that offer education to incarcerated adults, 43% of those who took part in education programs while incarcerated had a lower chance of re-offending than those who didn’t.
Comprehensive treatment considers the whole person rather than their disorder or illness. A person is made up of emotional, physical, environmental, and spiritual parts. It recognizes that individuals are complex beings with interconnected aspects of their lives and aims to treat the person as a whole rather than focusing solely on specific symptoms or conditions. The goal is to achieve balance and harmony within the individual by addressing all aspects of their well-being.
The holistic approach emphasizes the interconnectedness of the mind, body, emotions, and spirit, recognizing that imbalances in one area can affect other areas and contribute to various health issues or challenges. As shown above, the approach equips individuals with the necessary tools for sustained addiction recovery. From healthy coping mechanisms to stress management techniques to relapse prevention strategies, it empowers them to navigate challenges, make positive choices, and maintain their recovery over the long term.
Comprehensive treatment also emphasizes developing essential life skills like problem-solving, decision-making, and effective communication. This may, in turn, help reduce the risk of recidivism upon release. By prioritizing comprehensive treatment and support for individuals at risk of recidivism, we can make significant strides in breaking the cycle of addiction, reducing criminal behavior, and promoting healthier and more productive lives for those affected by substance abuse disorders.
Addiction is a complex disease that affects not only the mind but also the body. That's why addiction treatment must address an individual's whole body health. The holistic addiction treatment model takes into account the whole person - their physical, emotional, and spiritual well-being - rather than just treating the addiction itself. It recognizes that addiction is a complex issue that affects all aspects of a person's life and that successful treatment requires a comprehensive approach that addresses all of these aspects.
One key aspect of the holistic addiction treatment model is integrating exercise and nutrition into the treatment program. Exercise and nutrition can play a crucial role in supporting recovery from addiction. Exercise can help to improve physical health by promoting cardiovascular health, increasing muscle strength, and reducing the risk of chronic diseases such as obesity, diabetes, and heart disease. It can also help to alleviate symptoms of depression and anxiety, which are common co-occurring disorders among people with addiction.
Nutrition is also an essential component of holistic treatment. A healthy diet can help to support physical health, reduce the risk of chronic diseases, and improve mental health. Many people with substance use disorders have poor diets or unhealthy eating habits. Incorporating nutrition education and healthy food choices into addiction treatment can help to improve overall health and support recovery.
This article will examine how malnutrition and substance abuse go hand in hand. We’ll also cover the positive health benefits of exercise and eating a well-balanced, healthy diet, especially for those in the early stages of addiction recovery.

Exercise can be an effective tool in addiction recovery. It provides a range of physical, mental, and emotional benefits that can help individuals in the early stages of recovery manage the challenges and stressors that come with sobriety. Many treatment centers incorporate exercise into their programs for this very reason.
Substance abuse changes your mind and body chemistry. Even after treatment, you may still feel depressed, anxious, and sensitive to major stressors. But physical activity can help you shift the tide on those negative emotions.
In one study, regular swimming reduces the voluntary consumption of morphine in opioid-dependent rats. In another study, access to a running wheel reduces the self-administration of cocaine in cocaine-dependent rats.
Another small study analyzed an exercise program provided to 38 participants with substance use disorders. These participants agreed to participate in group exercises thrice weekly for 2-6 months. 20 participants finished the program. And in the follow-up a year later, 5 had maintained sobriety, and 10 said they had reduced their substance abuse.
Here's how exercise can help addiction recovery:
Exercise programs may include various activities like yoga, walking, swimming, or weightlifting, tailored to the individual's needs and interests.

Nutrition also plays a crucial role in early recovery from drug and alcohol abuse. Drugs and alcohol abuse can cause various nutritional deficiencies and digestive issues that can lead to both physical and psychiatric disorders. Therefore, it is essential to maintain a healthy and balanced diet to support the recovery process.
Here are some ways in which addiction can affect nutrition and diet:
Maintaining a balanced diet with whole foods, including complex carbohydrates, fruits, vegetables, lean proteins, and healthy fats, can provide the body with the necessary nutrients to support recovery. It is also crucial to avoid processed and sugary foods as they can lead to inflammation and other health problems. Healthy eating habits can:
Supplements may also be necessary to address specific nutrient deficiencies. Consulting a health care professional, like a nutritionist, can help determine your nutritional needs during recovery.
Needle exchange programs (NEPs) or syringe services programs (SSPs) are public health initiatives that provide clean needles and other injection equipment to people who inject drugs. They aim to reduce the transmission of blood-borne infections, such as HIV and hepatitis C, among drug users. NEPs also often offer other health services, such as:
Needle exchange programs provide needles and syringes to people who inject drugs. The program allows injection drug users to safely dispose of used needles and access new sterile ones. This helps reduce the spread of HIV/AIDS, hepatitis B and C, and other blood-borne diseases that can be transmitted through sharing or reusing needles. NEPs also provide additional services mentioned above.

NEPs are usually located in pharmacies, clinics, and organizations that provide health or community services. But the services can be delivered at fixed sites, outreach programs, mobile programs, and syringe vending machines.
Studies have shown that NEPs are extremely beneficial to public health. The Centers for Disease Control (CDC) shared a summary of information on the safety and effectiveness of SSPs, which included data from 30 years of research on the matter.
According to the report, comprehensive NEPs are safe, effective, and economical and don't promote crime or illegal drug use. In fact, new program users are 3x more likely to stop using drugs and 5x more likely to join addiction treatment than those who don't use SSPs. The report also points to the effectiveness of NEPs in reducing the transmission of HIV and other blood-borne diseases.
Beyond the CDC report, other bodies, including the United States Department of Health and the National Institute of Health, endorse the program's effectiveness in reducing HIV transmission and saving lives without losing ground in the battle against illegal drugs.
In addition to harm reduction, NEPs are cost-effective. They have reduced healthcare costs by preventing HIV, hepatitis, and other infectious diseases, including endocarditis. A 2014 analysis revealed that each dollar spent on syringe exchanges saves the government about $7 in HIV-related healthcare costs.
The programs have also effectively reduced dangerous conditions in the communities where they are implemented. They do this by providing addicts with a safe, healthy place to dispose of used needles, thus eliminating the need to discard them on streets or playgrounds. This helps keep neighborhoods cleaner and reduces the risk of injury from discarded needles.

NEPs are designed to reduce the spread of HIV/AIDS and other blood-borne diseases by providing a safe place for injection drug users to access sterile needles and dispose of used ones. This can help break the chain of transmission through sharing or reusing needles, as well as connect these individuals with substance abuse services.
Some argue that NEPs encourage substance abuse. But evidence from reputable sources, including the CDC, NIH, and Department of Health, shows that NEP does not promote drug use. The few cases indicating increased drug use should be analyzed to establish the circumstances under which negative effects might occur.
However, these scattered cases should not be used as a basis for discrediting the overall effectiveness of NEPs. These programs have reduced public health risks and provided a much-needed entry point into treatment and support services for people struggling with addiction.
Syringe services programs save lives by training drug users to prevent, quickly identify, and reverse opioid overdoses. Many NEPs give drug users and community members "overdose rescue kits" and educate them on how to recognize an overdose, give rescue breathing, and administer naloxone. Based on measures like hospitalizations for drug overdoses, there is no proof that community norms change in favor of drug use. For example, there were no increases in new drug users after the introduction of NEP in New Jersey, Hawaii, California, etc.
According to studies, NEPs protect the public and first responders by offering safe needle disposal and reducing the presence of needles in the community.

SSPs do more than improve health. Because they're so practical and far cheaper than the lifetime cost of treating HIV and viral hepatitis, they save taxpayers money. There have been a lot of politics surrounding the programs, with most states and local governments limiting or prohibiting SSPs. However, some restrictions have been lifted, providing further opportunities to assess their effects.
NEPs are effective at reducing the spread of HIV and other infectious diseases, promoting safe needle disposal, and providing access to evidence-based addiction treatments and support services. They are cost-effective and have been shown not to encourage drug use in the communities they serve. With proper implementation, NEPs can help reduce the burden of infectious diseases, drug use, and overdose-related deaths in communities worldwide.
No, needle exchange programs do not encourage drug use. Evidence from reputable sources,including the CDC and NIH, shows these programs are effective in reducing the transmission ofblood-borne diseases and increasing the likelihood of individuals seeking treatment withoutincreasing drug use. They also increase the likelihood that individuals will seek treatment forsubstance use disorders by providing access to healthcare services and support withoutpromoting the initiation or continuation of drug use.
Needle exchangeprograms offer several benefits to individuals who inject drugs, includingreducing the risk of transmitting blood-borne infections like HIV and hepatitis C by providingsterile syringes. They also offer access to health care services, substance use treatmentreferrals, and education on safer injection practices, contributing to overall public healthimprovement and harm reduction.
Yes, needle exchange programs significantly reduce healthcare costs bypreventing the spreadof infectious diseases like HIV and hepatitis C among people who inject drugs. By providingsterile needles and promoting safer injection practices, these programs decrease the incidenceof these costly-to-treat diseases, resulting insubstantial savings in healthcare expenses relatedto treating blood-borne infections.
Yes, needle exchange programs are legal in various parts of the United States, but their legalityand implementation can vary significantly by state and local jurisdictions. Some areas havefully endorsed these programs as part of public health strategies, while others may haverestrictions or do not have such programs in place.
Sleep disorders and addiction share a complex and bidirectional relationship. People who suffer from a sleep disorder may be more likely to abuse drugs or alcohol to try and self-medicate and achieve better sleep. For instance, they may use stimulant drugs to compensate for daytime fatigue caused by lost sleep.
In other cases, they may use drugs because of issues like cognitive impairment. Conversely, people addicted to drugs or alcohol may also suffer from sleep disorders due to the negative effects these substances can have on the body and mind.
There is a strong link between sleep disorders and addiction. A review by the Addiction Science & Clinical Practice found that about 70 % of patients admitted for detox had sleep issues before admission, and 80 % of those with sleep problems connect them to alcohol or illegal drug use.
According to the review, the relationship between the two seems to be bidirectional, with chronic or acute substance use disorders increasing the risk of developing sleeping problems. The review also adds that there's evidence indicating that long-term abstinence from chronic drug or alcohol use can reverse some sleep problems.
One of the most common ailments related to lack of sleep is depression. If you’re wondering whether or not you or someone you know suffers from depression, one way to learn more is to take a depression test.

Addiction is a brain disease. Chronic alcohol or drug use interferes with the brain, changing its chemistry and circuitry. These changes result in compulsive drug use and sleeping problems. Drug and alcohol use disorders can cause short- and long-term sleep issues like insomnia and sleep apnea.
Substance abuse also alters how a person through their sleep stages - messing up the rapid and non-rapid eye movement (REM and NREM). Generally, substance abuse can lead to:
Marijuana interacts with the endocannabinoid system (ECS) by binding to the cannabinoid receptors responsible for many roles, including regulating the sleep-wake cycle. This explains why more than 40% of those trying to quit marijuana experience sleeping problems. Many others experience sleep difficulty, strange dreams, and nightmares too.
Opioids like heroin bind to mu-opioid receptors, a body system that’s also responsible for sleep regulation. In fact, the name morphine or morphia, a medical derivative of opium, comes from Morpheus, the Greek god of sleep and dreams. Opioid drugs can induce sleepiness but also derange sleep by increasing transitions between different sleep stages.
Those going through withdrawal from heroin addiction can experience terrible insomnia. Opioids can also regulate respiration and, when taken in high doses, can severely impede breathing during sleep.
Depressants like alcohol may help people fall asleep, but they often lead to disruptions in sleep patterns and can make it difficult to stay asleep. Chronic alcohol use causes:
Stimulants like cocaine can make it difficult to fall asleep and cause people to wake up frequently at night. The sleep disturbances like insomnia and hypersomnolence mostly happen during cocaine intoxication and withdrawal. Other stimulants like amphetamine trigger dopamine release.

During acute administration, they can decrease total sleep time and sleep efficiency and increase sleep latency and the number of awakenings. In the withdrawal phase, there's a drop in sleep latency and a rise in total sleep time and efficiency.
Withdrawal from drugs can cause sleep disorders like insomnia, or other sleep problems, including restless legs syndrome, strange dreams, or broken sleep. These issues can take a toll on one’s physical and mental health, making a recovery harder. Sleep problems are common when withdrawing from:
Sleep disorders can also lead to substance abuse. Many people with sleep disorders turn to substances as a way to self-medicate or try and improve their sleep. For example:
As discussed earlier, people with sleep may take stimulants like caffeine, cocaine, or nicotine to stay awake during the day and then use alcohol or other drugs to fall asleep at night. Also, those struggling with addiction may disrupt their circadian system and end up with sleep disorders that lead them to use more substances to self-medicated. This can create a dangerous cycle in which they use substances to try and manage their sleep, but the substances themselves make it difficult for them to get the rest they need.
People who stop using drugs and alcohol often have better sleep. This happens because they are no longer disturbed by the side effects of those substances. When people get good sleep, they feel better and can concentrate more easily on their addiction recovery.
At the same time, people who sleep better don't need to use substances to cope with their fatigue. So, improving sleep can help break the cycle of addiction.
If you or a family member or someone you know is struggling with a sleep disorder and substance abuse, help is available. There are many treatment options that can address both issues at the same time. With treatment, it is possible to recover from both a sleep disorder and addiction.
The COVID-19 pandemic has been linked to increased drug overdoses across the United States. In fact, early data suggests that the number of overdose deaths in 2020 was higher than any previous year on record. According to the Centers for Disease Control, nearly 92,000 drug overdose deaths occurred in the US between May 2019 and May 2020. The CDC notes that although there was a rising trend in overdose deaths before the onset of the pandemic, the latest numbers show an increase in overdose deaths during the pandemic.
The overdose epidemic is a national public health crisis that has been exacerbated by the COVID-19 pandemic. It has led to widespread outbreaks of infectious diseases, such as HIV and hepatitis C, and numbers of deaths.
Overdose deaths from opioids have quadrupled since 1999, and in 2019 alone, over 49,000 people died from an opioid overdose. Synthetic opioids, particularly illicitly manufactured fentanyl, are responsible for the majority of these deaths.
Fentanyl is a powerful synthetic opioid that is 50 to 100 times more potent than heroin. In 2020, more than 56,000 overdose deaths involved synthetic opioids (other than methadone). This number accounted for 82% of all opioid deaths in that year.

The COVID-19 pandemic has only worsened the problem, as social distancing measures and lockdowns have led to increased drug use and overdoses. The pandemic also devastated the US economy, resulting in job losses and financial insecurity. This has led to increased stress and anxiety.
But overdose deaths aren't just limited to opioid use alone. The CDC notes that preliminary data shows increases in overdoses involving stimulants, such as methamphetamine and cocaine. In the 12 months ending in May 2020, there was a significant increase in the number of overdose deaths involving stimulants.
Overdose deaths increased significantly during the COVID-19 pandemic. In 2020, there were nearly 92,000 overdose deaths involving illicit drugs and prescription opioids. This rise in overdoses is driven by several factors, including:
Experts believe that the stress and anxiety of the pandemic have a big role in overdose deaths. Many people who struggle with substance abuse use drugs as a way to cope with difficult emotions and situations. The added stress of the pandemic can be overwhelming for someone who is already struggling, leading them to use more drugs than usual.
The pandemic has resulted in a decrease in access to treatment and recovery services. With fewer resources available, many people are unable to get the help they need. This can lead to a decline in sobriety and an increase in drug use.
The social isolation and loneliness caused by the pandemic can also lead to an increase in drug use. People who struggle with substance abuse often use drugs as a way to cope with negative emotions. The isolation of the pandemic can trigger these emotions, leading to an increase in drug use.

The COVID-19 pandemic has also had a profound impact on mental health. The CDC reports that adults aged 18-24 experienced the largest increase in mental health problems, such as anxiety and depression, during the pandemic. Mental health problems can lead to increased drug use and overdoses.
The pandemic has also resulted in a disruption in the supply of illicit drugs. The closure of borders and decrease in international travel has made it difficult for drug dealers to get their hands on illicit drugs. This has led to more dangerous substances being sold on the street.
Street drugs can be extremely dangerous for people who use illicit drugs, as it increases the risk of overdose. The disruption of the supply of illicit drugs also increased the price of drugs, which pushed some to cheaper alternatives, which could be more potent.
The coronavirus pandemic has also exacerbated racial disparities in drug overdoses. While the number of overdose deaths has increased, the increase has been highest among Black people. In 2020, there was a 44% overdose death rate among black people and 39% for Alaska Native and American Indians. White people had 22%.
The increase in deaths is largely driven by illicitly manufactured fentanyl. Blacks were more likely to die from an overdose involving fentanyl.

According to the National Institute on Drug Abuse, overdose deaths have been on the rise in the United States for the past two decades. But the numbers increased sharply during the pandemic. The opioid epidemic has had a devastating effect on families and communities across the country, and it is clear that something needs to be done to prevent further tragedy. Here are some things that can be done to prevent overdose deaths:
· One way to reduce the number of overdose deaths is to increase access to treatment for substance abuse disorders. This includes everything from prevention and early intervention programs to specialized treatment facilities.
· Additionally, it is important to increase access to naloxone, a medication that can reverse the effects of an opioid overdose. Naloxone is available without a prescription in many states, and it can be administered by family members or bystanders.
By increasing access to treatment and naloxone, we can start to turn the tide on the opioid epidemic and prevent more lives from being lost to overdose.
The COVID-19 pandemic has had a devastating impact on the lives of people struggling with addiction. Any ground gained in harm reduction for drug addiction in the last few years was overwhelmed by COVID-19. The isolation and loneliness of the pandemic, as well as the disruption in the supply of illicit drugs, have led to an increase in drug use and overdoses. Racial disparities in overdose deaths have also been exacerbated by the pandemic.
If you or someone you love is struggling with addiction, it is important to get help as soon as possible. Addiction treatment can save lives.
If you have, at any point in your life, interacted with drug addicts, you are likely aware of just how far they would go to ensure they get their high any time they want. Even though they are addicts, they go out of their way to conceal their drugs from other people.
They may go to great lengths when hiding a stash, using creative and sometimes elaborate methods, like hiding them in body cavities, such as the rectum or vagina, stashing them in hollowed-out books or other objects, or wearing multiple layers of clothing to create hidden pockets. In some cases, addicts may even swallow condoms filled with drugs in an attempt to smuggle them into a treatment facility or detox center.
However, these methods are not foolproof, and addicts often eventually get caught. If you suspect that someone you know is struggling with addiction, look for signs of drug paraphernalia or hidden stash spots. You can also look for changes in behavior, such as secrecy, lying, or unexplained absences. Your loved one can be creative, but if you look close enough, you’ll uncover any addiction behaviors and help they get the help they need.
This article reveals the common ways addicts conceal their drugs. If you are worried that your loved one is abusing drugs, read on to see where they may be hiding their illicit drugs or drug paraphernalia.

The dangers of drug addiction are well-known, but the ways in which addicts hide their drugs might surprise you. One popular method is called "stash clothing." Deep pockets or interior pockets is the most common way to hide the drugs in the clothes. You can also hide in sleeve or sewn into clothing. The advantage of this method is that it allows addicts to keep their drugs close at hand without being obvious about it.
But sometimes, addicts may take it a notch higher. For example, some women hide their marijuana stash in altered tampons and hairbands. Those who work in transporting illegal drugs can sew the drugs in wigs and have the wigs glued to their heads to go past border and customs without being suspected. Unfortunately, doing so may cause complications and necessitate emergency room electrolysis.
Let us discuss a little more about how addicts hide contraband in clothing and footwear.

You would be surprised at how many different places addicts hide their stash, especially at music festivals. They know the consequences of drug possession, so they need to ensure they don’t get caught. No one wants to spend time in jail, not even them.
They roll the contraband into jeans, sew them into jacket linings, or hide them in coin pockets or socks. Unfortunately, addicts or smugglers that have children conceal the contraband in their kids’ clothing, hoping that the officers won’t search the children. Those with babies hide them in baby blankets.
Since police officers realized that coin pockets are a popular hiding place, young adults became more cunning. They either buy clothes with hidden pockets or opt to make the hidden pocket themselves.
Addicts’ demand for clothes with hidden compartments made entrepreneurs mass-produce clothes that can easily conceal drugs. These clothes are readily available on the internet, and they are relatively famous for cocaine storage and hiding weed.
It is rather unfortunate that some brands specialize in clothing for carrying drugs. These clothes are sold online and in stores. Some of the most popular garments for stashing drugs include
These are just a few examples of mass-produced clothing addicts use to stash their drugs. Although the clothes may not have been made explicitly for drug hiding, they are famous for their ability to hide contraband properly, and some articles promote them as such.
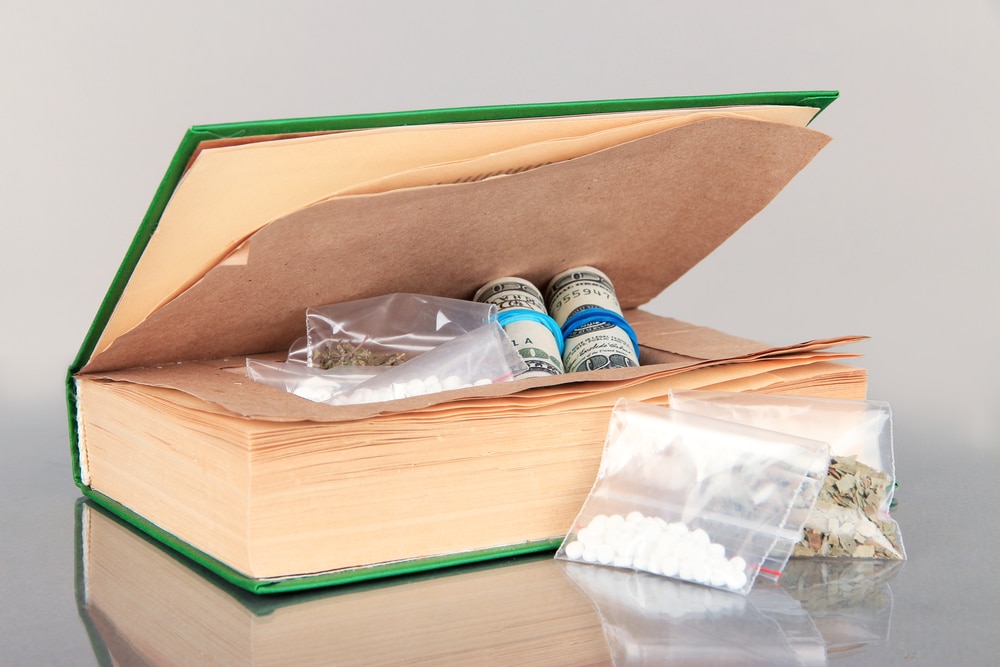
As discussed above, addicts can be very creative with hiding their drugs. Other than hiding them in their clothing and footwear, they may also hide them in:
Addicts are always secretive about where they hide their drugs. But by knowing the common hiding spots, you can uncover their behavior and help them get the care they need.
Over the last two decades, people have normalized combining different drugs to achieve a more intense high. It is not uncommon to see an individual mixing alcohol with a prescription drug or psychoactive and psychedelic substances. If someone uses drugs sold on the street, the chances are that this person drinks alcohol too.
Most drug addicts are unaware of the severe short-term and long-term effects of illegal drug combinations. This article discusses hippie flipping, candy flipping, and polysubstance abuse.
Polysubstance use refers to consuming more than one drug at once. When you engage in polysubstance use, you get a more pronounced feeling from consuming illicit drugs.
Most users have a drug of choice that they combine with other drugs to enhance the effect of their primary drug.
Unfortunately, those diagnosed with polysubstance abuse are usually addicted to the feeling of being high using multiple drugs.
Polysubstance abuse may increase the effects of the drugs, but it also has severe adverse effects that most drug abusers are unaware of.
Hippie flipping and candy flipping are the most common forms of polysubstance abuse.

Several factors contribute to polysubstance abuse, including:
Polysubstance abuse has severe long-term and short-term effects. When you combine drugs, the side effects increase exponentially.
The effects also tend to be more potent than those of individual drugs. As a result, you are likely to have acute health problems, and your chances of overdose are much higher. Treatment of Polysubstance abuse is also complicated.
Hippie flipping, also called flower flipping, refers to using psilocybin mushrooms and MDMA simultaneously.
When you hippie flip, you will experience a psychedelic and euphoric trip. Hippie flipping is quite common in clubs and other social settings.

The effects of hippie flipping depend on:
Since the above factors determine the effects of hippie flipping, the effects vary from individual to individual. However, the constant is a mosaic of different sensations and emotions.
Possible side effects are:
The length of your hippie flip depends on how you timed the two doses. The effects of MDMA last for 3-6 hours, while mushroom’s effects last for 4-6 hours. For this reason, a hippie flip can last for anywhere between 6 and 12 hours. However, some people report experiencing side effects like headaches and lethargy two days after hippie flipping.
Like most drug combinations, mixing mushrooms and MDMA has serious risks. MDMA can cause serotonin syndrome, resulting in high body temperature, cardiac arrhythmia, and muscle cramping. On the other hand, mushrooms prevent serotonin reuptake from your brain cells; thus, the drugs remain in your system for much longer.
Mushrooms and MDMA can potentially damage brain cells since they over-activate the cells. Other additional side effects include nausea, weakness, dry mouth, jaw clenching, insomnia, extreme thirst, dizziness, rapid eye movement, and more.
If you start by taking psychedelic mushrooms before MDMA, you will likely have a standard MDMA crash at the end, which includes feelings of anxiety and extreme sadness. If you take the mushrooms last, the hallucinogenic effects of mushrooms may mask the MDMA crash. Although most hippie flippers prefer this, it often creates conditions for a bad trip. Most hippie flippers report that they feel spent and tired during the comedown.
Candy flipping refers to mixing LSD and MDMA. MDMA, commonly sold as ecstasy in pill form, is a psychoactive drug, while LSD, commonly known as acid, is a psychedelic drug.
Most people that candy flip start with LSD then follow it up with MDMA after approximately 4 hours. This way, they feel the peak effects of LSD first, then follow it up with the feel-good vibes of MDMA.

The effects and intensity of candy flipping vary from individual to individual. You may even experience different effects every time you candy flip. For this reason, it is challenging to say what its exact outcome will be.
Most candy flippers claim they experience intense MDMA-like effects, but others claim they experience the effects of both substances in equal measure.
According to the National Institute on Drug Abuse, common MDMA effects include:
Common LSD effects include:
The candy flipping experience lasts for 12-24 hours because LSD effects last for 12 hours,
and MDMA effects last for 3-6 hours.
Candy flipping presents several severe and potentially dangerous risks. Besides the effects mentioned above, you may have a bad trip and hydration issues.

Candy flipping has an unpleasant comedown. The possible comedown effects are:
You may also experience paranoia and depression. These comedown effects may last for several days.
Mixing drugs and alcohol or different kinds of drugs increases your risk of harmful and potentially dangerous side effects. Besides the side effects discussed above, you will likely develop substance use disorders.
If you or your loved one are struggling with hippie flipping, candy flipping, or polysubstance abuse, it would be best to seek professional help. Several treatment programs are available, and you can choose one that suits you best.
A lot can happen when you take more than the usual or recommended dose of a drug. Sometimes, you could experience mild symptoms like loss of coordination. But in extreme cases, you may end up with severe, harmful symptoms or even death. This is called an overdose.
Usually, your body’s metabolism can get rid of the substance, neutralizing the harmful effects. But if the drug level exceeds the threshold that your body can metabolize, the drug’s side effects can harm you physically and mentally.
An overdose happens when you take a toxic amount of a medicine or drug. It can be intentional or accidental:
According to the Centers for Disease Control, there have been 841,000 drug overdose deaths since 1999.

In 2019 alone, 70,630 overdose deaths happened in the US. Of this number, about 70% involved an opioid, mainly synthetic opioids. Cocaine, on the other hand, accounted for 15,000 overdose deaths in the US in 2017. The misuse of and addiction to opioids is a crisis that affects public health.
The most recent data by the Centers for Disease Control and Prevention reveals that about 100,306 people died from a drug overdose in the US during the 12 months ending April 2021.
An overdose is a medical emergency that needs immediate medical attention. Seek medical advice if you exhibit the following symptoms after taking a drug, alcohol, or a combination of both. You can also call 911 for urgent cases.
With that in mind, let’s look at what happens to your body when you overdose.
What happens to your body when you overdose?
When you overdose, chances are you won’t be aware of what’s happening. However, those around you will spot some or all of the symptoms discussed above. Usually, that’s because of how the drugs interact with your body.

When you overdose on opioids, your body temperature, heart rate, and breathing may drop to dangerously low levels, causing suffocation, heart attack, or brain damage. Your veins may collapse and suppress the normal flow of blood throughout the body. You may also find it hard to spit or swallow because of the suppression of the gag reflex.
Opioid overdose may disrupt the normal functioning of receptors between the heart and brain, leading to slow heart rate or no heart rate at all. Slow breathing translates to low oxygen levels and abnormal heart rhythms.
Opioids may also limit oxygen flow to the brain and cause permanent brain damage within four minutes of oxygen deprivation. They may cause seizures that further damage the brain. In extreme cases, this damage can leave you paralyzed and unable to speak.
Overdosing on stimulants or overamping causes the opposite symptoms to overdosing on opioids. Patients experience chest pain, passing out, irregular breathing, racing heart, sweating, feeling hot, high blood pressure, weakness, shaking, or stroke. Overdosing to cocaine is particularly bad and can cause stroke or heart attack.
Other things that might happen when you overdose:

There are different treatments for a drug overdose. Your doctor will determine the right one for you based on the type of drugs involved and symptoms. They may:
You’ll need to see a doctor for a follow-up to ensure no delayed injuries to any body organ. If it was an intentional overdose, follow-up also ensures that there are systems in place to prevent a recurrence.
Once a deliberate overdose is managed and you are out of immediate medical danger, you’ll need psychiatric care. You may also be considered for a mental health evaluation. Getting support for mental or substance abuse problems can be helpful.
If it’s a child, they’ll need help dealing with the trauma and learning from the mistake. A follow-up can reduce anxiety and educate the child and the parent.
Keep all medications in a safe and secure place to prevent accidental overdose. In case it’s an unintentional, illicit drug overdose, it’s best to get away from access to the drugs to prevent the problem from recurring.
If it’s an intentional overdose, you’ll need to address the underlying problem fast. Addiction treatment can help reverse the effects of substance abuse and get you on the path to recovery.