In the intricate web of human relationships, the interplay between love and addiction emerges as a profoundly complex and often misunderstood dynamic. At the heart of countless families and partnerships, addiction casts long shadows, challenging our notions of love, commitment, and mutual support. This blog post seeks to delve into the nuanced relationship between addiction and love, shedding light on why an addict may struggle to express love in ways that are healthy, consistent, or recognizable to their loved ones. The significance of understanding this dynamic cannot be overstated, as it holds the key to fostering empathy, patience, and resilience in the face of a condition that can deeply fracture bonds and erode the fabric of intimacy and trust.
Addiction, characterized by the compulsive use of substances or engagement in behaviors despite adverse consequences, is a chronic brain disorder that alters the very architecture of desire and reward. This alteration can profoundly impact an individual's emotional landscape, decision-making processes, and, crucially, their ability to love and be present for others. As we explore the reasons "why an addict can't love you," it's essential to approach the topic with compassion and a deep understanding of addiction's grip on the mind and soul of those it ensnares.
Furthermore, this discussion is not merely academic but serves as a beacon of hope and understanding for those navigating the turbulent waters of a relationship affected by addiction. Whether you're seeking answers, solace, or strategies to bridge the gap that addiction has created in your relationship, this blog post aims to offer insights and perspectives that can light the path toward healing and understanding. In examining the complexities of love and addiction, we invite readers to engage with an open heart, ready to explore the depths of human connection and the potential for recovery and renewal within the grasp of every individual touched by addiction.
The concepts of love and addiction, while fundamentally different, share a complex relationship that can blur the lines of dependency and affection. To navigate the intricacies of how addiction impacts relationships, it is essential first to define these terms separately, providing a clear foundation for understanding their interplay.
Love is a profoundly multifaceted emotion, often described as an intense feeling of deep affection towards another person. It encompasses a range of positive emotional and mental states, from the deepest interpersonal affection to the simplest pleasure. Love involves elements of care, closeness, protectiveness, attraction, and trust. It is the glue that binds individuals together, enabling them to navigate life's challenges as a cohesive unit. However, the subjective nature of love makes it a complex emotion to define universally, as it encompasses various dimensions, including familial, platonic, and romantic love, each with its unique characteristics and expressions.

Addiction, on the other hand, is a chronic brain disorder characterized by compulsive engagement in rewarding stimuli despite adverse outcomes. It significantly affects the brain's system of reward, motivation, and memory. People suffering from addiction are overwhelmingly focused on obtaining and using substances or engaging in behaviors that provide them with a sense of relief or euphoria, often at the expense of their health, relationships, and responsibilities. This compulsive behavior is driven by an altered brain chemistry that prioritizes the addiction above all else.
The complexities of defining love are further compounded when examining behaviors associated with addiction. Addiction can mimic certain aspects of love, such as the intense focus on the object of one's addiction, which parallels the focus one might have on a loved one. However, whereas love seeks the well-being and happiness of the other, addiction is inherently self-serving, seeking gratification through substance use or behaviors that lead to detrimental consequences for the individual and their relationships.
Understanding these definitions is crucial as we delve into the reasons why an addict may struggle to offer the emotional presence, consistency, and support that are hallmarks of a loving relationship. The behaviors associated with addiction disrupt the ability to maintain these attributes, challenging the very essence of what it means to love and be loved in return.
One of the primary reasons "why an addict can't love you" lies in how addiction profoundly distorts an individual's emotional landscape. Addiction's grip on the brain extends far beyond a mere craving for substances or engagement in compulsive behaviors; it fundamentally alters the brain's chemistry and neural pathways. This alteration affects the person's ability to experience, regulate, and express emotions in a healthy manner. Emotions, under the influence of addiction, become hijacked by the relentless pursuit of the addictive substance or behavior, leading to a distorted perception of priorities, values, and, critically, relationships.
The emotional distortion created by addiction means that an addict often experiences a narrowed emotional range, primarily focused on the highs of the addiction or the lows of withdrawal. This skewed emotional experience leaves little room for the nuanced emotions that foster deep, meaningful connections, such as empathy, compassion, and unconditional love. The addict's emotional bandwidth is consumed by the addiction, impairing their ability to genuinely connect with others and express love in a way that is recognizable and fulfilling to their loved ones.
This impairment is not a reflection of the addict's desire or capacity to love but rather a tragic consequence of addiction's all-consuming nature. It underscores the necessity of addressing the underlying addiction to restore emotional availability and the capacity to engage in healthy, loving relationships.
Addiction often takes center stage in an addict's life, consuming their thoughts, time, and resources. This overwhelming focus on obtaining and using substances or engaging in addictive behaviors leaves little room for anything else, including relationships. The prioritization of addiction above all else means that loved ones are often sidelined, as the addict's need for the substance or behavior overshadows their ability to maintain and nurture their relationships. This shift in priorities can lead to neglect, broken promises, and a general absence in the moments that matter, eroding the foundation of trust and intimacy that love requires. The sad reality is that, in the throes of addiction, the addict may seem to choose their addiction over their loved ones, not because they don't care, but because the addiction controls their decision-making processes.
Addiction leads to a form of emotional numbing, where the addict becomes increasingly detached from their feelings and those of others. This emotional detachment is a coping mechanism, helping the addict avoid the guilt, shame, and pain associated with their addiction. However, it also means they are less present and emotionally available for their loved ones. Relationships thrive on emotional exchange and vulnerability, which are severely compromised when one partner is unable to engage emotionally. This lack of emotional availability creates a barrier to forming deep, meaningful connections, making it challenging for an addict to participate in a loving relationship fully.

Feelings of guilt and shame are common among addicts, stemming from their actions while under the influence or as they grapple with the consequences of their addiction. These emotions can be overwhelming, leading to a cycle of continued substance use as a way to escape or numb these feelings. The cycle of guilt and shame not only perpetuates the addiction but also hinders the addict's ability to engage in healthy relationships. The burden of guilt and shame can make an addict feel unworthy of love, pushing them further into isolation and preventing them from opening up to and connecting with their loved ones. This cycle creates a significant barrier to love, as it prevents the building of trust and intimacy that are essential for a loving relationship.
Addiction can have a devastating impact on an individual's financial stability, often leading to significant financial strain on relationships. The cost of sustaining an addiction, coupled with potential job loss and decreased productivity, can deplete a family's resources, leading to stress and conflict within the relationship. Financial insecurity may force loved ones into positions of hardship and sacrifice, further straining the relationship. When financial issues dominate a relationship's dynamics, it becomes challenging to focus on the emotional aspects of love, as survival and stability become the primary concerns. This strain not only undermines the sense of security and support that love provides but also diverts attention and energy away from nurturing the relationship, making it difficult for an addict to show love in the ways that matter most.
Despite the formidable challenges that addiction imposes on relationships, there remains a profound potential for healing and renewal. This journey towards recovery and reconciliation emphasizes the critical roles of compassion, understanding, and structured support, not only for the addict but also for their loved ones. The question of "can a drug addict truly love someone" transitions from a query mired in doubt to a beacon of hope as individuals and families navigate the path of healing together.
Central to this healing process is the recognition of addiction as a disease that requires professional treatment and a supportive environment to overcome. Rehabilitation programs, therapy, and support groups offer the addict a foundation for recovery, addressing the underlying issues driving the addiction and providing strategies for managing its challenges. Concurrently, loved ones can engage in their healing journey, often through therapy and support networks like Al-Anon, which offer guidance in coping with the emotional turmoil and practical challenges posed by addiction. Healing also involves the gradual rebuilding of trust and emotional connection, aspects of the relationship that are deeply eroded by addiction. This reconnection does not occur overnight but through consistent, honest communication, mutual effort, and the re-establishment of boundaries and trust. It's in these moments of vulnerability and shared struggle that the capacity for love, often obscured by the haze of addiction, begins to resurface.
Moreover, the role of compassion cannot be overstated—compassion for the self and for each other. Understanding that relapse can be a part of the recovery journey, and maintaining a stance of empathy and support through setbacks, underscores the belief in the possibility of change.
As families and couples navigate these challenges, the question shifts from "can an addict love you" to "how can we foster love in the face of addiction?" It's a journey that underscores the resilience of the human spirit and the transformative power of love, understanding, and support in overcoming the shadows cast by addiction.
In the End
In exploring the intricate dynamics between love and addiction, we've delved into the reasons why addiction can so profoundly impact an individual's capacity to engage in healthy, loving relationships. From the emotional distortion and prioritization of addiction over relationships to the barriers created by financial strain, guilt, and shame, the challenges are significant. Yet, within these challenges lies a thread of hope—a potential for healing that underscores the resilience of both the human spirit and the bonds that connect us.
This journey through the complexities of love in the shadow of addiction highlights not just the struggles but also the profound possibilities for recovery and renewal. It reaffirms that, while addiction may temporarily obscure an individual's ability to love and be present, it does not erase their fundamental capacity for connection and affection. With compassion, understanding, and the right support, there is a pathway to rekindling the depth and authenticity of these connections.
The discussion we've embarked upon serves as a beacon for those navigating the turbulent waters of relationships affected by addiction. It's a reminder that the question is not so much "can an addict love you," but rather "how can we navigate and heal from addiction together?" Love, in its most resilient form, has the power to transcend the barriers erected by addiction, offering hope for a future where relationships are not defined by the struggle but by the strength found in overcoming it together.
As we conclude, let this exploration serve as an invitation to view relationships through a lens of empathy and understanding, recognizing the challenges but also embracing the potential for healing and growth. In doing so, we can transform the narrative from one of despair to one of hope, support, and, ultimately, love.
REFERENCES
Table of Contents
In our journey through life, the paths we take are as varied and complex as the reasons behind our choices. Among these, the decision to use drugs stands out as a particularly intricate issue, fraught with emotional, societal, and biological underpinnings. At Struggling With Addiction, we recognize the multifaceted nature of drug use and addiction, and it's our mission to explore these layers with an authoritative yet compassionate lens. This article delves into the question, "Why do people use drugs?"—a query that opens the door to understanding not just the act of drug use itself but the human experiences that often precede it.
Drug use does not occur in a vacuum; it is influenced by a tapestry of factors, from the pressures of one's social environment to internal battles with mental health. By exploring the reasons behind drug use, we aim to shed light on the myriad pathways that can lead individuals to this critical point. This understanding is crucial, not only for those who find themselves on this path but also for their loved ones seeking to offer support and guidance. Through a compassionate exploration of why people turn to drugs, we hope to foster empathy, awareness, and, ultimately, healing.
Understanding drug use requires a nuanced look at the myriad factors that lead individuals to engage with substances that can alter their state of consciousness. Drug use spans a broad spectrum, from casual and experimental use to chronic abuse and addiction, each with distinct motivations and implications. It's crucial to distinguish these categories, as not all drug use leads to addiction, yet the potential for substance use disorders remains a significant risk.
At its core, drug use is a behavior influenced by a confluence of societal, psychological, and biological factors. Societally, the environment in which an individual lives can significantly impact their exposure to and attitudes towards drugs. Cultural norms, peer influences, and socio-economic conditions play pivotal roles in shaping one's propensity to use drugs. Psychologically, individuals may turn to drugs as a means to cope with stress, emotional pain, or mental health disorders. The temporary escape drugs offer from reality can be alluring, especially in the absence of healthier coping mechanisms.
"Addiction begins with the hope that something 'out there' can instantly fill up the emptiness inside." – Jean Kilbourne
https://hawaiianrecovery.com/rehab-blog/our-20-favorite-addiction-quotes
Biologically, genetics and brain chemistry contribute to an individual's susceptibility to addiction. Certain individuals may have a genetic predisposition that increases their risk of developing substance use disorders. Additionally, drugs can hijack the brain's reward system, creating a cycle of craving and compulsion that can be difficult to break.
Understanding these factors is not about assigning blame but about recognizing the complexity of drug use. By acknowledging the diverse influences that lead individuals to use drugs, we can approach the issue with empathy and develop more effective support and treatment strategies. This comprehensive view underscores the importance of addressing not only the symptoms of drug use but also its root causes, paving the way for more holistic interventions.
Lets explore the major reasons why people use drugs:
The psychological underpinnings of why individuals turn to drugs are as varied as they are profound. Central to many of these reasons is the desire to escape—be it from stress, emotional turmoil, or the haunting memories of trauma. For many, drugs offer a temporary reprieve from the relentless pressure and pain of their daily lives. Both reasons add to a significant increase in the percentage of people who struggle with addiction. This search for relief is a powerful motivator, leading individuals down a path where the solution to their problems seems to lie in the very substances that can ultimately exacerbate them.
Mental health disorders play a significant role in this dynamic. Conditions such as depression, anxiety, and post-traumatic stress disorder (PTSD) can greatly increase the likelihood of drug use. For those battling these issues, drugs can seem like a viable method to dull the sharp edges of their psychological pain. However, this relief is often fleeting, and the cycle of dependence and addiction can worsen the very symptoms individuals seek to mitigate.
The pursuit of pleasure, too, is a psychological factor driving drug use and a possible reason why many people deny their addictions. The brain's reward system, designed to reinforce life-sustaining activities, can be hijacked by the artificial highs drugs provide. This pursuit can quickly spiral into addiction, as the brain's chemistry and structure are altered, leading to an increased tolerance and a relentless craving for more.
Understanding these psychological factors is crucial for addressing drug addiction compassionately and effectively. It highlights the need for mental health support as an integral part of addiction treatment, recognizing that the battle against addiction is not only physical but deeply rooted in the psychological struggles individuals face. This approach fosters a more holistic understanding of drug use, emphasizing the importance of addressing both the symptoms and the underlying emotional and mental health issues.
Psychological factors play a pivotal role in why individuals turn to drugs, often serving as a conduit through which people seek relief from their internal struggles. The labyrinth of human emotions and mental health conditions can make individuals more susceptible to the allure of substance use as they navigate the complexities of their psychological pain. Mental health disorders such as depression, anxiety, and post-traumatic stress disorder (PTSD) are particularly significant, acting as both catalysts and accelerators for drug use. For those grappling with these conditions, drugs can present a misleading escape hatch, offering a temporary solace from the relentless torment of their minds.
The relationship between psychological distress and drug use is cyclical and reinforcing. Drugs may provide a momentary easing of psychological pain, but this relief is often ephemeral, leading to a deeper entrenchment of both the mental health issue and the substance dependency. This cycle is further complicated by the fact that the initial reasons for drug use, such as coping with stress or trauma, can be overshadowed by the addiction itself, creating a new set of psychological challenges.
Moreover, the pursuit of pleasure and the brain's reward system play significant roles in drug use. The powerful highs produced by drugs can seem irresistible, especially against the backdrop of emotional or psychological pain. This pursuit, however, is fraught with danger, as it can lead to a dependency that alters the brain's chemistry, making natural sources of pleasure seem insufficient by comparison.
Addressing the psychological factors behind drug use requires a compassionate, multifaceted approach that includes mental health support as a cornerstone of addiction treatment. By understanding and treating the underlying emotional and psychological issues, individuals can find more sustainable paths to recovery, breaking the cycle of addiction and fostering a deeper, more lasting healing.
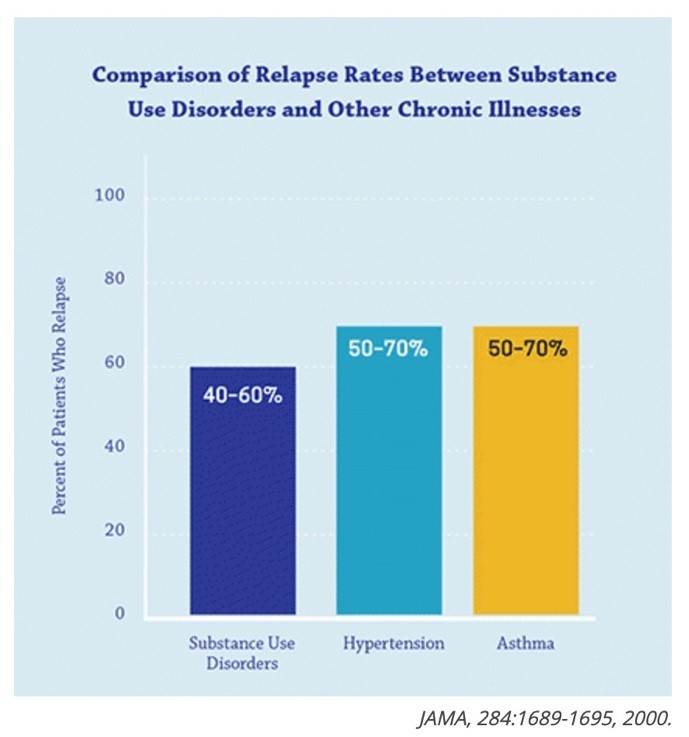
Biological and genetic factors significantly contribute to the complexity of drug use and addiction, underscoring the reality that vulnerability to addiction can be inherited. Research has shown that genetics can account for approximately 40% to 60% of an individual's susceptibility to addiction. This genetic predisposition, combined with environmental influences, can greatly increase the risk of developing substance use disorders. The interplay between genes and environment highlights the nuanced nature of addiction, where biology sets the stage, and life experiences can cue the onset of drug use and subsequent addiction.
Moreover, the brain's biochemistry plays a critical role in the addiction process. Drugs can profoundly alter the brain's reward system, creating a cycle of intense cravings and compulsive drug use. These substances mimic the brain's natural chemicals but have much more potent effects, leading to changes in brain function over time. This alteration not only affects an individual's ability to experience pleasure naturally but also impacts decision-making, stress regulation, and self-control.
Understanding addiction as a brain disease helps to dismantle the stigma associated with drug use. It emphasizes the need for medical and therapeutic interventions that address the biological aspects of addiction. Recognizing the biological underpinnings of addiction fosters a compassionate approach to treatment, focusing on the individual's health and recovery rather than a moral failing.
Curiosity and the innate human desire for experimentation often serve as gateways to drug use, particularly among adolescents and young adults. This exploratory behavior is a natural part of development, driven by a quest for new experiences and the challenge of societal boundaries. However, when this curiosity intersects with drug use, it can lead to unforeseen consequences, including the potential for addiction. The allure of experiencing something novel or the desire to feel different from one's usual self can be compelling reasons why individuals, especially the youth, are drawn to drugs.
Experimentation with drugs is often influenced by peer dynamics, where the pressure to conform or the desire to be accepted plays a crucial role. In social settings where drug use is normalized or glamorized, the threshold for trying drugs can be significantly lowered. This normalization can mask the inherent risks associated with drug use, leading individuals to underestimate the potential for harm and addiction.
The critical factor in this stage of drug use is the lack of foresight regarding the long-term implications. What begins as a casual experiment can quickly evolve into regular use, as individuals chase the initial highs they experienced. This transition from experimentation to habitual use underscores the importance of early intervention and education. By providing young people with accurate information about the risks of drug use and fostering environments that encourage healthy coping mechanisms, it's possible to mitigate the impact of curiosity-driven experimentation.
Addressing the curiosity and experimentation that often lead to drug use requires a balanced approach that respects individual freedom while emphasizing the importance of informed decision-making. Through supportive dialogues and preventative measures, society can help individuals navigate their curiosity in ways that promote well-being and safety.
The use of drugs as a coping mechanism for life's challenges is a significant factor behind substance abuse. Many individuals turn to drugs in an attempt to manage stress, alleviate pain, or escape from the realities of their circumstances. Life events such as trauma, loss, and chronic stress can overwhelm an individual's ability to cope, pushing them towards substances that offer temporary relief. This form of self-medication, however, often leads to a perilous cycle of dependence and addiction as the temporary solace provided by drugs fades, necessitating increased consumption to achieve the same effect.
"Drugs are a waste of time. They destroy your memory and your self-respect and everything that goes along with your self-esteem." – Kurt Cobain
Understanding drug use as a coping strategy requires a compassionate response that addresses the root causes of distress. It's crucial to acknowledge that behind every instance of drug use as a coping mechanism, there lies a deeper story of struggle and pain. Effective intervention strategies should focus not only on the substance use itself but also on developing healthier coping skills and resilience. By offering support, resources, and alternative strategies for managing life's challenges, individuals can be guided towards more constructive means of dealing with their problems, reducing the reliance on drugs as a temporary escape. This approach not only aids in combating addiction but also in healing the underlying emotional and psychological wounds that fuel substance use.
The accessibility and availability of drugs play a crucial role in their use and the subsequent development of addiction. In communities where drugs are readily obtainable, the likelihood of initial use and eventual dependency increases significantly, as does drug overdose. This ease of access can transform casual or experimental use into a persistent habit, as obtaining substances becomes a simple matter of convenience. Moreover, the rise of prescription drug misuse highlights another dimension of accessibility; medications intended for legitimate medical use can become gateways to addiction when not used as prescribed or when they fall into the hands of individuals for whom they were not intended.
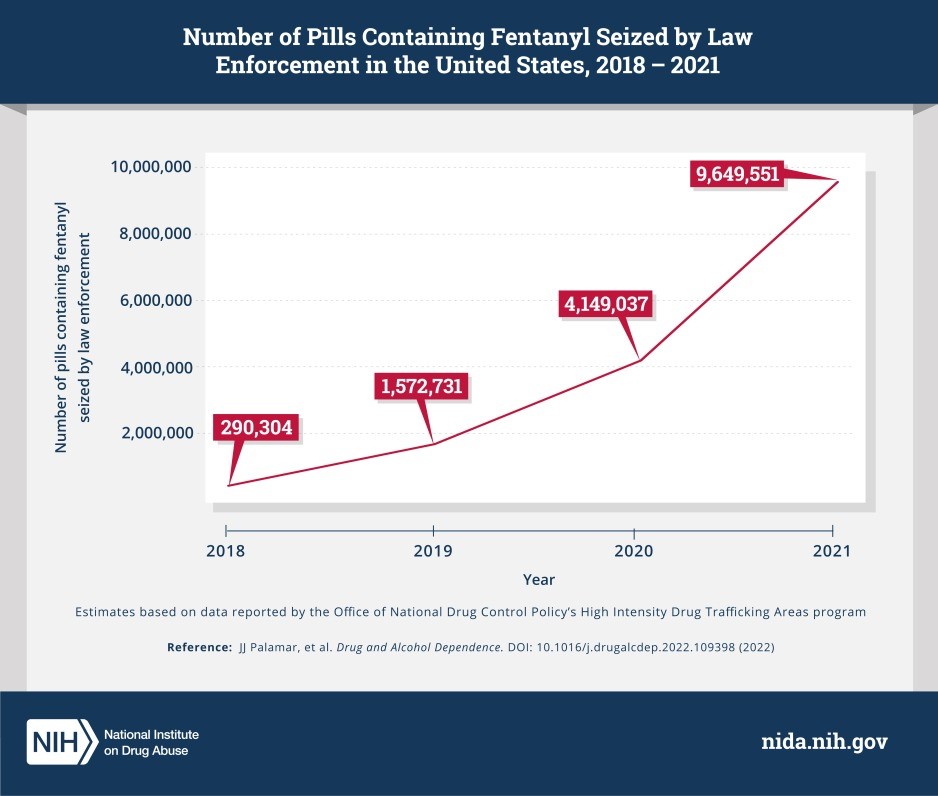
Addressing the challenge of accessibility requires a multi-faceted approach that includes stricter regulation of prescription drugs, education on the risks of misuse, and community-based initiatives aimed at reducing the availability of illicit substances. Equally important is the need to provide accessible and effective treatment options for those seeking to overcome addiction. By creating environments where drugs are harder to obtain and support is easier to access, the cycle of drug use and addiction can be disrupted.
Efforts to combat the accessibility and availability of drugs must be balanced with compassion and support for individuals struggling with addiction, recognizing that punitive measures alone are not sufficient to address the underlying issues. Providing pathways to recovery and support systems for those affected is essential in creating a holistic approach to reducing drug use and its associated harms.

In exploring the multifaceted reasons why people use drugs, we uncover a complex tapestry of societal, psychological, biological, and personal factors. Each narrative of drug use is as unique as the individual, yet common threads weave through these stories, revealing the shared human experience of seeking relief, escape, or pleasure. Understanding these motivations is crucial for addressing the challenges of drug addiction with empathy, compassion, and effectiveness.
Our journey through the reasons behind drug use underscores the importance of holistic approaches to addiction treatment and prevention. It highlights the necessity of addressing not only the physical aspects of addiction but also the emotional, psychological, and environmental factors that contribute to it. By fostering environments that promote healthy coping mechanisms, offering support for mental health, and ensuring access to comprehensive treatment options, we can make strides in reducing the prevalence and impact of drug use and addiction.
As we conclude, let us remember that behind every statistic and every case of drug use, there are individuals with stories, struggles, and the potential for recovery. By approaching drug use with understanding and compassion, we can offer hope and support to those on the path to recovery, contributing to a healthier, more supportive society for all.
Sources:
Table of Contents:
In the journey of parenthood, witnessing your teenager struggle with drug addiction is profoundly distressing. The path to recovery is intricate, demanding a thoughtful decision when selecting a teen drug rehab center. The importance of this choice cannot be overstated, as the right environment can significantly alter the course of your teenager's future. This guide is dedicated to parents navigating these turbulent waters, aiming to provide an authoritative yet compassionate roadmap to making an informed decision tailored to your teen's unique needs.
Teenage years are a critical period marked by rapid physical, emotional, and social development. During these formative years, teenagers are especially vulnerable to the allure of drug use due to various factors, including peer pressure, the desire for experimentation, and coping mechanisms for stress or mental health issues. Recognizing the signs of addiction and understanding the necessity of early intervention is the first step toward healing. However, the process of choosing a drug rehab center for teenagers is fraught with questions and uncertainties.
How do you assess your teen's specific needs? What treatment approaches are most effective for adolescents? How can you navigate the complexities of insurance coverage and manage the cost of rehab? This article aims to address these pivotal questions, offering guidance to parents committed to finding a rehabilitation facility that not only addresses the physical aspects of addiction but also nurtures the emotional and psychological well-being of their teenager. Through this guide, we endeavor to support you in making a decision that paves the way for a healthier, drug-free future for your child.
Understanding teen drug addiction requires a compassionate yet realistic perspective, acknowledging the unique challenges adolescents face in today's society. Teenagers are in a critical phase of their lives, where they encounter rapid changes physically, emotionally, and socially. These changes can make them more susceptible to drug use as they seek to navigate stress, peer pressure, and the quest for identity. The allure of drugs often lies in their perceived ability to offer an escape from the pressures of adolescence or to fit in with a particular social group.
Teen drug addiction is not merely a phase or a result of poor decision-making; it's a complex interplay of factors, including genetics, environmental influences, and mental health issues. Many teens struggling with addiction also suffer from co-occurring disorders such as depression, anxiety, or trauma-related conditions. This duality complicates their path to recovery, necessitating a treatment approach that addresses both the addiction and the underlying mental health issues.
Early detection and intervention are crucial in preventing the escalation of drug use into a full-blown addiction. Recognizing the signs of drug abuse—changes in behavior, academic performance, physical health, and social circles—is the first step towards helping your teen. Understanding addiction as a disease that can affect any teenager, regardless of background, is vital. This perspective fosters empathy and support, guiding parents to seek professional help that can offer their teenager the best chance for a successful recovery.

Assessing your teen's specific needs before choosing a drug rehab center is a crucial step that requires careful consideration and, often, professional guidance. Every teenager's journey into addiction is unique, influenced by a myriad of factors such as the type of substance used, the length and intensity of use, underlying mental health conditions, and individual personality traits. Understanding these nuances is essential in selecting a rehab facility that aligns with your teen's specific circumstances and maximizes the chances of successful recovery.
The assessment process begins with an honest and open conversation with your teen to understand their perspective and willingness to seek help.
"The Goal Isn’t To Be Sober. The Goal Is To Love Yourself So Much That You Don’t Need To Drink." – Author Unknown
However, given the complexity of addiction, enlisting the help of a professional—such as a psychologist, psychiatrist, or addiction specialist—is highly recommended. These professionals can conduct comprehensive evaluations to identify the severity of the addiction, any co-occurring mental health disorders (such as depression or anxiety), and the teen's overall physical health.
This evaluation should also consider the teen's learning style, social skills, and interests to ensure that the rehab program can offer engaging and effective treatment modalities. For example, a teenager who responds well to creative expression might benefit from a program that includes art or music therapy.
Moreover, assessing your teen's specific needs also involves understanding the family's role in the recovery process. Family dynamics, the availability of support systems, and the willingness to participate in family therapy sessions can significantly influence the treatment's effectiveness.
Ultimately, choosing a drug rehab center for your teenager is not about finding a one-size-fits-all solution but identifying a program that can tailor its approach to meet your teen's individual needs, fostering a path to recovery built on understanding, care, and personalized support.
Finding the right teen drug rehab center is a pivotal step towards ensuring a supportive and effective recovery journey for your adolescent. This process involves thorough research, careful consideration of various factors, and, often, consultations with professionals. Key criteria to keep in mind include the center's accreditation, the qualifications of its staff, its treatment philosophy, and the specific services it offers.
Accreditation by recognized healthcare organizations guarantees that the facility meets high standards of care and treatment practices. Equally important is the expertise of the staff, including addiction specialists, therapists, and counselors, who should have experience working with teenagers and understand the unique challenges they face.
The treatment philosophy of the center should align with your teen's needs. Some centers focus on holistic recovery, incorporating physical, emotional, and spiritual wellness, while others may emphasize evidence-based therapies such as cognitive-behavioral therapy or family therapy. It's crucial to select a rehab that offers a comprehensive approach, addressing not just the addiction but also any co-occurring mental health issues.
Moreover, consider the type of programs available, such as inpatient versus outpatient, the length of treatment, and aftercare support. Facilities that offer a continuum of care, from detoxification to aftercare planning, can provide a more seamless and supportive recovery experience.
Lastly, involve your teen in the decision-making process as much as possible. Their willingness to participate in a particular program can significantly influence their recovery outcome. Selecting the right drug rehab center is a collaborative effort, aiming to find a place where your teen feels safe, supported, and motivated to embark on the path to recovery.

Navigating insurance coverage and managing the costs associated with teen drug rehab can be a daunting aspect of finding the right treatment program for your child. Understanding the intricacies of insurance benefits and exploring financial assistance options are critical steps in ensuring that your teenager receives the necessary care without placing undue financial strain on the family.
Start by thoroughly reviewing your health insurance policy to determine what types of addiction treatment services are covered. Many insurance plans, especially those compliant with the Affordable Care Act, provide coverage for substance abuse treatment to some extent. However, coverage can vary widely in terms of types of treatment covered (e.g., inpatient, outpatient, counseling), duration of treatment, and out-of-pocket costs. Contact your insurance provider directly to get detailed information about your teen's eligibility for rehab services, including any pre-authorization requirements or preferred providers that may affect coverage.
If insurance coverage is limited or non-existent, don't lose hope. Many rehab centers offer sliding scale fees based on family income or payment plans that allow you to spread the cost over time. Additionally, some facilities may have scholarships or grant programs available to help offset costs for families in need. It's also worth exploring state and federal assistance programs that offer support for addiction treatment.
Remember, investing in your teenager's recovery from drug addiction is crucial. While the financial aspect of rehab can be overwhelming, focusing on finding a treatment program that offers effective, personalized care for your teen should be the priority. Taking the time to research and understand your options can lead to more manageable costs and a successful start to your child's journey to recovery.
When evaluating prospective rehab centers for your teenager, asking the right questions is essential to determine if a facility is the best fit for your child's needs. These inquiries can provide deep insights into the center's approach, effectiveness, and compatibility with your teen's situation. Here are key questions to consider:
Asking these questions will help you gauge the center's commitment to providing high-quality, adolescent-focused care and support, ensuring you make a well-informed decision for your teenager's recovery journey.
Supporting your teen through rehab is a critical component of their recovery journey, requiring patience, understanding, and active participation from the family. As your teenager embarks on this challenging path, your role as a parent is to provide unwavering support and encouragement, reinforcing the importance of the treatment process and the positive changes it brings.
"Being in recovery has given me everything of value that I have in my life." – Rob Lowe
Firstly, educate yourself about addiction and the recovery process. This knowledge will help you empathize with your teen's struggles and communicate more effectively. Be an active participant in family therapy sessions if offered by the rehab center. These sessions are valuable for repairing relationships, improving communication, and understanding the dynamics that may contribute to your teen's substance use.
Maintain open lines of communication with your teen, showing that you are a source of unconditional love and support. Listen to their fears, frustrations, and hopes without judgment. Encourage them to express their feelings and be honest about their recovery journey.

Lastly, create a supportive home environment that promotes sobriety. This might include setting clear expectations, establishing healthy routines, and removing any triggers that could hinder their recovery. Celebrate milestones and acknowledge the efforts your teen is making toward recovery, reinforcing the idea that every step forward is an achievement worth recognizing.
By providing a solid foundation of support, you play a crucial role in your teenager's path to recovery, helping them navigate the challenges of rehab and emerge stronger and more resilient.
In navigating the complex journey of selecting the right teenage drug rehab center, it's essential to approach the process with patience, diligence, and an open heart. The path to recovery for your teenager is paved with challenges, but with the right support and drug rehab information, a future free from addiction is within reach. By thoroughly assessing your teen's specific needs, understanding the effective treatment approaches, and finding a rehab center that aligns with these criteria, you are laying the groundwork for a successful recovery. Moreover, navigating the financial aspects thoughtfully and asking the right questions during your search will ensure that you choose a facility that not only meets your child's immediate needs but also supports their long-term well-being.
Supporting your teen through the rehab process and beyond is a testament to your unwavering love and commitment to their health and happiness. Remember, recovery is a journey that doesn't end with rehab; it requires ongoing support, understanding, and encouragement. Celebrate the small victories, remain steadfast during setbacks, and keep the lines of communication open.
Choosing the right teen drug rehab center is a significant decision, but you don't have to make it alone. Seek guidance, lean on professionals, and remember that this guide is here to support you every step of the way. With the right approach, resources, and drug addiction information, you can provide your teenager with the best possible chance for a healthy, drug-free future.
Pain management is one of the most significant healthcare crises in the US, with nearly 50% of Americans visiting physicians with a primary complaint of pain each year. It can be acute and short-lived or chronic when it lasts for months or years. Pain can affect a person's quality of life and make it hard to work.
Pain management aims to safely minimize pain and increase your ability to do everyday activities. Healthcare providers may employ various methods to achieve this, including prescription painkillers, commonly known as opioids. Opioids are among the most potent tools in the arsenal against pain. These drugs have been used for centuries to alleviate suffering, but their use hasn't been without risks and controversy.
Opioids, a class of drugs that includes prescription painkillers like oxycodone, hydrocodone, and morphine, are often a go-to solution for managing moderate to severe pain. Healthcare providers prescribe opioids for various reasons, including:
Opioid medications work by binding to specific receptors in the spinal cord and brain, altering the perception of pain. While they are highly effective in providing relief, opioids come with a substantial risk of addiction.

Opioids are highly addictive because they hijack the brain's natural reward system, creating a robust association between drug use and pleasurable sensations. When introduced to the body, opioids interact with specific receptors and trigger the release of neurotransmitters, particularly dopamine, in the brain's reward pathway.
Dopamine is associated with pleasure, reward, and reinforcement of enjoyable experiences. Therefore, its increased release heightens the sense of pleasure and euphoria and reinforces the association between opioid use and positive feelings.
Opioids not only activate the reward system but also effectively alleviate pain by modulating pain signals in the brain and spinal cord. The dual effect of pain relief and euphoria makes opioids particularly appealing to those experiencing both physical and emotional distress. However, the repeated association between opioid use and pleasure creates a habit, and the brain begins to crave the drug.
Responsible opioid use can turn into drug dependency due to various factors, including:
Opioids are often prescribed for short-term pain management. However, in some cases, when pain persists, patients may continue to use opioids for an extended period. Prolonged use increases exposure to opioids, which can cause changes in the brain's chemistry and heighten the risk of dependence.
Tolerance is a physiological adaptation where the body becomes accustomed to the presence of opioids, requiring higher doses to achieve the same level of pain relief. As a result, one may gradually escalate their opioid use. Increased tolerance can occur even with responsible use, mainly when opioids are used over an extended period. This can contribute to a cycle of higher doses, which in turn heightens the risk of developing dependency.
Regular follow-ups and assessments are crucial to evaluate the effectiveness of the treatment, assess pain levels, and identify any signs of misuse or dependence. If healthcare providers do not closely monitor a patient's response to opioids and make necessary adjustments to the treatment plan, there's a risk of the patient inadvertently developing dependence.
Chronic pain often coexists with psychological factors such as stress, anxiety, or depression. Opioids not only provide pain relief but also may temporarily alleviate emotional distress. Individuals may unintentionally start using opioids for emotional relief, contributing to the development of psychological dependence. Using prescription opioids to self-medicate is a form of substance abuse and can result in addiction or overdose.
Lack of patient education about the risks of opioid use and the importance of adhering to prescribed doses can contribute to dependency. Patients must understand the potential consequences of prolonged use and the importance of following the prescribed treatment plan.
The initial prescribing practices play a critical role. Overprescribing, prescribing high doses, or prescribing opioids without a precise treatment plan can contribute to the development of dependency. Responsible prescribing involves a careful assessment of the patient's needs, consideration of non-opioid alternatives, and ongoing monitoring.

Here are some real stories and case studies from real people who shared their accounts about dealing with prescription opioids. The CDC initially published these stories.
Ann Marie's story is a tragic illustration of the devastating progression of prescription opioid addiction. Her son Christopher, a talented 20-year-old baseball player, was prescribed opioids for back pain after being involved in a minor accident. But his tolerance escalated quickly, leading him to seek out multiple doctors willing to prescribe more of these powerful medications.
Over a short period, Christopher's opioid intake soared from one pill a day to a staggering 25 pills a day. This rapid escalation is a clear sign of the development of dependence and addiction. The opioids took a toll on his physical health and also had a profound impact on his overall well-being. Everything he had once valued, including family, academics, and his passion for baseball, began to lose importance.
Christopher's behavior underwent a drastic transformation. He struggled with sleep, frequently stayed out at night, and became defensive and combative towards his loved ones. Recognizing the severity of her son's addiction, Ann Marie attempted to get him into various treatment facilities.
Unfortunately, Christopher faced rejection or expulsion due to his poor behavior. Sadly, Christopher's addiction progressed, and two years later, he fatally overdosed. Ann Marie started Christopher's Reason to help direct those struggling with opioid addiction to the treatment they need.
19-year-old Britton got prescription opioids for a severe shoulder injury that he sustained while serving in the US Army. But by age 22, he was addicted. His addiction was compounded by his relationships with fellow Veterans who misused prescription opioids and his wife's substance use disorder.
In the 11 years that he struggled with opioid use disorder, Britton separated from his wife, who later died due to drug use complications, and lost custody of his children. He was even arrested and jailed in 2018.
Britton attributes his recovery to the structured therapy program. He is now remarried and raising his children. He hopes that his story will help demonstrate that opioid use disorder can happen to anyone and that there's help for those facing the disease.

Many non-opioid approaches are available to help manage pain. These therapies and treatment options can help alleviate pain and minimize the need to depend solely on opioids for pain relief:
Prescription opioids are an essential part of pain management, especially in situations where pain is severe or difficult to control through other means. When used responsibly and under the vigilant support and supervision of healthcare professionals, opioids can provide effective relief for many different types of pain. The collaboration between patients and healthcare providers is fundamental for the success of pain management.
The connection between pain management and opioid addiction lies in the use of prescription opioids to treat pain. Opioids are highly effective at relieving pain but also carry a high risk of addiction and dependence. Individuals prescribed opioids for pain management, especially over an extended period, may develop tolerance, requiring higher doses to achieve the same pain relief. This escalation in dosage increases the risk of opioid dependence and addiction.Moreover, opioid medications can produce feelings of euphoria and relaxation, making them attractive to individuals seeking to escape from emotional or psychological distress. As a result, some individuals may misuse or abuse opioids, leading to addiction. Additionally, chronic pain conditions and co-occurring mental health disorders, such as depression or anxiety, can further increase the vulnerability to opioid addiction.Overall, while opioids can be effective in managing pain when used appropriately, their addictive potential underscores the importance of careful prescribing practices, close monitoring, and the consideration of alternative pain management strategies to mitigate the risk of opioid addiction.
Opioids are a class of drugs used primarily for their pain-relieving properties, including prescription medications like oxycodone, hydrocodone, and morphine, as well as illegal drugs like heroin. They alleviate pain by binding to opioid receptors in the brain, spinal cord, and other areas of the body, blocking the transmission of pain signals and reducing the perception of pain. Additionally, opioids can induce feelings of euphoria and relaxation by affecting areas of the brain associated with reward and pleasure, contributing to their potential for misuse and addiction.
While opioids can be highly effective for managing acute or severe pain, their use carries risks such as tolerance, dependence, and addiction. Therefore, it's essential to use opioids judiciously, under the supervision of a healthcare professional, and to explore alternative pain management strategies whenever possible to mitigate the risk of opioid-related harms.
Yes, there are several alternative pain management strategies that can help reduce the risk of opioid addiction. These include non-opioid medications such as non steroidal anti-inflammatory drugs (NSAIDs), acetaminophen, and certain antidepressants or anticonvulsants, which can be effective for managing certain types of pain. Physical therapy, occupational therapy, and chiropractic care can also be beneficial, as they focus on improving mobility, strength, and flexibility, which can help alleviate pain and reduce reliance on opioids. Additionally, complementary and alternative therapies such as acupuncture, massage therapy, mindfulness-based stress reduction, and yoga have shown promise in managing chronic pain and may be effective as part of a comprehensive pain management plan. By incorporating these alternative strategies into treatment plans, healthcare providers can provide patients with safer and more effective options for pain management while minimizing the risk of opioid addiction.
Common relapse triggers that individuals may encounter include stress, which can arise from various sources such as work, relationships, or financial difficulties. Negative emotions such as anxiety, depression, or loneliness can also trigger cravings for substances as individuals seek relief from emotional distress. Social triggers, such as being around people who use drugs or being in environments associated with past substance use, can also increase the risk of relapse. Additionally, certain cues or reminders, such as seeing drug paraphernalia, visiting places where drugs were used, or experiencing sensory triggers like smells or tastes associated with drug use, can elicit cravings and prompt individuals to relapse. By identifying these common triggers, individuals in recovery can develop strategies to cope with them effectively and reduce the risk of relapse.
The modern gaming industry has gone through a dramatic transformation over the past few decades, evolving from a niche hobby into an entertainment juggernaut. With the advent of powerful gaming consoles, PC gaming, and the proliferation of smartphones, gaming has become an integral part of global culture. Video games today are not just about entertainment; they are a thriving economic sector, an art form, and a social space where millions of players interact and compete.
However, amid this growth, there are growing societal concerns of microtransaction addiction. Microtransactions are small, often in-game purchases that players make to enhance their gaming experience. These purchases can range from cosmetic items like skins and outfits to gameplay-affecting items like weapons or power-ups. Although microtransactions offer players a way to personalize their gaming experience, they have also raised concerns about their potential to lead to addictive behaviors.
Many digital games have adopted paid reward systems and in-game currency that allow players to buy game-specific content. With approximately 3.09 billion active gamers worldwide, paid reward systems like in-game purchases, card packs, loot boxes, and battle passes have become an incredibly lucrative business model for game developers and publishers. According to PwC, the global digital games market is worth 257.1 billion in 2023 and is expected to reach 321.1 billion by 2026. Of this number, in-game purchases stand at approximately $61 billion, accounting for the largest slice of the global gaming market.
Despite this growth, a recent study from Loughborough and Newcastle universities found that items obtained from microtransactions were harmful, especially to young people and vulnerable consumers. In fact, the research found that young people who purchased loot boxes had a higher risk of becoming gamblers or developing problem gambling than others.
A loot game is a chance-based game that includes a randomized selection of in-game items that can only be seen after the loot box opens. It can go by different names, including card packs, mystery boxes, bags, eggs, gifts, wishes, cookie cutters, spins, etc., which makes it difficult for young people, parents, and carers to recognize them as games of chance. Players earn or buy loot boxes with real-world money. These loot boxes contain:
Other studies also linked excessive gaming to psychiatric disorders like anxiety and depression, as well as addictive behaviors. This is primarily due to games introducing gambling-like mechanisms. For instance, gamers can use real money to gamble at the Diamond Casino and Resort in the Grand Theft Auto V (GTA-5) video game. The nature of gaming has also changed with the rise of smartphones, allowing gamers to play games on the go while providing Freemium options (that are free and premium). Freemium games are free to play but offer in-game purchases for real money.
Microtransaction addiction is characterized by players compulsively spending real money on in-game purchases, often to the detriment of their finances, well-being, and personal relationships. This addiction can create a pattern strikingly similar to traditional gambling patterns, with players chasing the thrill of acquiring virtual items or progressing in the game through these pay-to-play actions. As microtransactions become more prevalent in the gaming industry, the concern surrounding their addictive nature has escalated.

When individuals engage in activities that result in pleasurable experiences, like making in-game purchases and receiving rewards, it activates the brain's reward pathways, primarily involving the release of the neurotransmitter dopamine. Over time, repeated activation of these pathways reinforces the association between the activity (making a microtransaction) and the pleasurable outcome (receiving a reward).
With continued engagement in microtransactions, the brain can become sensitized to the pleasurable effects. This means that over time, one may require more frequent or larger rewards to achieve the same level of pleasure. As a result, they may engage in even more microtransactions to chase that initial sense of satisfaction.
The brain's neural connections adapt based on behavioral patterns. If making microtransactions becomes a habitual behavior, the neural pathways associated with this behavior can become strengthened. This reinforces the inclination to engage in the same behavior repeatedly, even when it may not be in the individual's best interest.
Neuroplastic changes in the brain can lead to the development of cravings and compulsive behaviors. As the brain associates microtransactions with pleasurable outcomes, it can generate cravings for those experiences. Cravings, in turn, can drive individuals to engage in microtransactions even when they consciously recognize the negative financial and psychological implications.
Neuroplasticity can also affect decision-making processes. Over time, the brain may prioritize the immediate pleasure derived from microtransactions over long-term considerations, such as financial impact, relationships, etc. This shift in decision-making can contribute to the cycle of addiction.

In-game purchases, particularly those involving loot boxes and other chance-based microtransactions, can create patterns of behavior similar to traditional gambling addictions. For one, they leverage reward mechanisms to keep players engaged. The intermittent reinforcement schedule, where players receive rewards at unpredictable intervals, is a hallmark of both traditional gambling and loot boxes. This unpredictability can lead to players repeatedly making purchases in the hope of receiving valuable items.
There’s also the Fear-Of-Missing-Out (FOMO) aspect, where players fear missing out on limited-time offers, exclusive items, or events. Game developers use these strategies to create a sense of urgency and drive compulsive purchasing behaviors. In many cases, they also showcase the purchases of other players to create a competitive environment where players may feel pressured to spend more to keep up with others. This can lead to unhealthy financial decisions driven by social comparison.
Sadly, once a player has invested a significant amount of money into microtransactions, they may develop a sunk-cost fallacy. This cognitive bias makes them feel compelled to continue spending to justify their previous investments, even when it becomes financially detrimental. To make matters worse, human psychology is wired to be loss-averse, meaning people are more motivated to avoid losses than to gain equivalent rewards. When players invest money in microtransactions and don't receive the desired items, they may perceive it as a loss and feel compelled to spend more to avoid further "losses."
Microtransaction addiction can have significant and wide-ranging impacts on individuals, affecting their mental, emotional, and financial well-being:
The Federal Trade Commission Act takes action against video game companies that engage in unfair or deceptive practices. Better Business Bureau’s National Advertising Division (NAD) does the same thing, reviewing advertisement claims for accuracy and truthfulness. NAD aims to protect children from potentially unfair practices related to microtransactions. But still, there is a real potential for players to experience harm in relation to microtransactions, especially since there aren’t any specific gaming regulations that govern chance-based outcomes.If you or someone you know is struggling with microtransaction addiction, don't hesitate to reach out for help. There are plenty of addiction resources and treatment options available to help you regain control of your life and find healthier ways to enjoy gaming and entertainment.
Addiction thrives in the shadows of unconscious behaviors and automatic responses. Mindfulness exposes these patterns, allowing you to better understand your cravings, triggers, and emotional undercurrents that drive addictive behaviors. That’s why mindfulness is considered critical in addiction recovery. This article explores the profound impact of mindfulness on addiction recovery and how you can harness it to create lasting change.
Mindfulness is the practice of intentionally paying attention to the present moment without judgment or distraction and with an attitude of curiosity and acceptance. It involves being fully aware of your thoughts, feelings, bodily sensations, and the surrounding environment without trying to change or evaluate them.
Mindfulness emphasizes focusing on the here and now rather than dwelling on the past or worrying about the future. It involves fully engaging with your current experience, whether it's through your breath, senses, or immediate surroundings.
You can practice mindfulness through meditative practices like:

The human brain is the only organ that’s shaped by practice and experience. This means that when you repeatedly engage in specific behaviors and thoughts, your brain reorganizes itself by forming new neural connections. This is how addictions happen – when you repeatedly engage in addictive behaviors like substance abuse, your brain adapts to the behavior by strengthening the neural connections related to it.
Mindfulness practices work much the same way and help you to create new neural connections and strengthen existing ones that support present-moment awareness, self-regulation, and non-reactive observation. This process can counteract the neural pathways associated with addictive behaviors by redirecting attention away from cravings and habitual responses.
Both addiction and mindfulness leverage the brain's capacity for neuroplasticity. However, they lead to vastly different outcomes.
Neuroscientific studies have shown that regular mindfulness practices can lead to structural and functional changes in the brain, particularly in regions associated with attention, emotion regulation, and self-awareness.
Mindfulness encompasses several key components that work together to cultivate a mindful mindset. These components include:
Mindfulness plays a crucial role in rewiring the brain. According to the American Psychological Association, mindfulness gives you control over your thinking, allows you to disengage from emotional reactions, and more effectively self-regulate. As you continue to engage in mindfulness practices, you strengthen neural pathways associated with healthier coping mechanisms and emotional regulation. This process gradually weakens the neural connections linked to addiction, making it easier to resist cravings and maintain sobriety.

Mindfulness is increasingly recognized as a valuable tool in addiction recovery due to its positive impact on various aspects of physical, mental, and emotional well-being. Here's how mindfulness helps in addiction recovery and why you should leverage these meditation benefits for a better life:
Mindfulness encourages you to become acutely aware of your thoughts, emotions, bodily sensations, and cravings. This heightened self-awareness is crucial in addiction recovery because it helps you recognize triggers, patterns of behavior, and the early signs of cravings.
Mindfulness equips you with techniques to manage and regulate your emotions. When cravings or stress arise, you can use mindfulness practices to remain calm and centered. You learn to acknowledge your feelings without judgment, reducing the urge to turn to substances or addictive behaviors as a way to cope.
Addiction often involves impulsive actions driven by cravings. Mindfulness helps you pause and create space between your impulses and actions. This pause allows you to consider the consequences of your choices and make more deliberate decisions.
Mindfulness teaches you to approach cravings with curiosity and acceptance rather than resistance. You learn to observe cravings as passing mental events, understanding that they will eventually subside. This reduces the intensity and duration of cravings, making them easier to manage.
Addiction recovery can be stressful, and stress is a common trigger for relapse. Mindfulness practices, such as deep breathing exercises and meditation, provide effective recovery tools to reduce stress and promote relaxation. By incorporating mindfulness into your daily routine, you can better cope with the challenges of recovery.
Addiction often leads to a scattered and preoccupied mind. Mindfulness exercises, such as mindfulness meditation, train your mind to focus on the present moment. This improved concentration can help you stay on track with your recovery goals and avoid distractions that may trigger relapse.
Mindfulness fosters resilience by helping you develop a non-judgmental attitude toward yourself. You become more compassionate and forgiving, reducing feelings of shame or guilt that can hinder recovery. This resilience enables you to bounce back from setbacks and maintain your commitment to sobriety.
Mindfulness practices, such as Mindfulness-Based Relapse Prevention (MBRP), are specifically designed to prevent relapse. MBRP helps you recognize high-risk situations, cope with cravings, and implement mindful strategies to maintain your sobriety.
Beyond addiction recovery, mindfulness enhances your overall well-being. It promotes a sense of inner peace, contentment, and a deeper connection to yourself and others. This positive shift in your mental and emotional state can motivate you to stay committed to a sober and fulfilling life.
Incorporating mindfulness into your daily routine and treatment plan can be a valuable asset in your journey toward lasting recovery. It provides you with practical tools to navigate the challenges of addiction and promotes a sense of empowerment and self-mastery.
Mindfulness practices offer significant benefits for individuals in addiction recovery. By cultivating mindfulness, individuals can develop greater self-awareness, allowing them to observe their thoughts, emotions, and physical sensations without judgment.This heightened awareness enables individuals to recognize triggers for substance use and implement healthier coping strategies to manage cravings and avoid relapse.
Additionally, mindfulness promotes stress reduction and emotional regulation, essential skills for navigating the challenges of recovery. Techniques such as mindfulness meditation, deep breathing exercises, and body scans help individuals alleviate feelings of anxiety, depression, and emotional distress commonly experienced during recovery. Furthermore, practicing mindfulness fosters acceptance and compassion toward oneself and others, fostering a positive mindset and greater resilience in the face of adversity. Integrating mindfulness into addiction recovery supports long-term sobriety, enhances overall well-being, and empowers individuals to thrive on their journey toward wellness.
Yes, there are specific mindfulness-based interventions and programs designed specifically for addiction recovery. One well-known program is Mindfulness-Based Relapse Prevention(MBRP), which integrates mindfulness practices with cognitive-behavioral techniques to prevent relapse and promote sustainable recovery. MBRP teaches individuals in recovery how to apply mindfulness skills to recognize and cope with cravings, manage stress and difficult emotions, and cultivate greater self-awareness and acceptance. Through a structured curriculum of mindfulness meditation, psycho education, and group discussions, participants learn practical strategies for maintaining sobriety and enhancing overall well-being.
Another example is Mindfulness-Based Stress Reduction (MBSR), a program developed by Jon Kabat-Zinn that teaches mindfulness meditation and stress reduction techniques to promote physical and mental health. While not specifically designed for addiction recovery, MBSR has been adapted and integrated into substance abuse treatment programs to address stress-related triggers and support recovery. Additionally, other mindfulness-based interventions, such as Acceptance and Commitment Therapy (ACT) and Dialectical Behavior Therapy (DBT),incorporate mindfulness practices as part of a comprehensive approach to treating addiction and co-occurring mental health disorders. These programs provide individuals in recovery with practical tools and skills to navigate the challenges of addiction and cultivate a greater sense of well-being and resilience.
Individuals in recovery can seamlessly integrate mindfulness into their daily routines to bolster their journey toward sobriety and overall well-being. Beginning the day with a brief mindfulness practice, such as a mindful breathing exercise or a body scan meditation, sets a positive tone and cultivates a sense of presence for the day ahead. Throughout their daily activities, individuals can infuse mindfulness by consciously engaging in routine tasks with full attention and intention, such as eating mindfully or walking with awareness of each step.These moments of mindfulness foster a deeper connection to the present moment and promote greater clarity and focus.
Moreover, individuals can incorporate mindfulness into moments of stress or craving by pausing to observe their thoughts and emotions without judgment. Practicing grounding techniques, like focusing on the breath or the sensations in the body, helps individuals manage stress and maintain emotional balance during challenging situations. Regular mindfulness breaks scattered throughout the day serve as opportunities to reset and recenter, fostering resilience and enhancing overall well-being. Finally, ending the day with a mindfulness practice, such as a guided meditation or gratitude reflection, promotes relaxation and prepares individuals for restful sleep, ensuring they recharge and rejuvenate for the day ahead. By weaving mindfulness into their daily routines, individuals in recovery empower themselves with valuable tools for managing stress, cultivating resilience, and nurturing their sobriety journey.
Several mindfulness resources and apps cater to individuals in addiction recovery, providing accessible tools and practices to support their journey toward sobriety and well-being. Headspace is a popular app offering guided meditations, mindfulness exercises, and sleep aids tailored to reduce stress, enhance focus, and foster relaxation. Similarly, Calm and marisagrieco.com provide a diverse range of meditation programs, breathing exercises, and relaxation techniques designed to alleviate anxiety, improve sleep quality, and cultivate mindfulness in daily life. Insight Timer offers a vast library of guided meditations, music tracks, and talks from mindfulness teachers worldwide, allowing users to customize their meditation experience based on their preferences and needs.
Moreover, individuals can explore mindfulness-based programs such as Mindfulness-BasedStress Reduction (MBSR) or Mindfulness-Based Relapse Prevention (MBRP), available in local communities or online platforms. These structured courses offer guidance and support for integrating mindfulness into addiction recovery, promoting emotional regulation, stress management, and relapse prevention. Additionally, many addiction treatment centers and mental health organizations incorporate mindfulness-based practices into their recovery services, providing group sessions, workshops, or individual therapy that incorporate mindfulness techniques. By utilizing these resources and programs, individuals in addiction recovery can develop essential mindfulness skills to navigate challenges, promote well-being, and sustain long-term sobriety.
Nicotine pouches are among the fastest-growing nicotine delivery products in the US. According to data, nicotine pouch dollar sales increased by 470% over the first half of 2020. People are drawn to them due to their discreet nature, availability of flavors, and the perception of reduced harm compared to traditional tobacco products.
Nicotine pouches are particularly appealing to those concerned about the adverse effects of smoking and seeking alternative methods to satisfy their nicotine cravings. The absence of smoke and tobacco leaf in nicotine pouches gives users the impression that they are making a safer choice.
But what many people don't know is that nicotine pouches still contain nicotine. In fact, their nicotine concentration levels are comparable to moist snuff and snus and often exceed levels found in nicotine replacement therapy products. As such, transitioning from smoking to using nicotine pouches can mean inadvertently trading one addiction for another.
This article will discuss the hidden dangers of nicotine pouches and provide steps to quit their use.
Nicotine pouches are small, dissolvable microfiber pouches pre-filled with nicotine salt powder, flavorings, and sweeteners. They are designed to deliver nicotine to the user without smoking or chewing tobacco. They are typically placed between the gum and lip, where they slowly release nicotine into the bloodstream through the oral mucosa.
Some popular brands of pouches include Zyn, Velo, and On!, and they come in colorful packaging that looks like mint containers. Note that nicotine and toxin levels vary significantly from brand to brand. For example, Zyn products, which are among the most popular in the market, have nicotine levels of up to 6mg per pouch.

The safety of nicotine pouches is a topic that requires careful consideration. While they are often marketed as a potentially safer alternative to smoking, it is essential to recognize that the long-term effects of this nicotine delivery method are still largely unknown.
The FDA classifies nicotine pouches as smokeless tobacco products rather than smoking cessation devices or pharmaceutical products. This classification means that they are not regulated as strictly as smoked tobacco products, such as cigarettes.
The lack of stringent regulation and the limited research on pouches contribute to the challenge of determining their safety. The scientific community has not yet gathered sufficient long-term data to fully understand the potential health risks associated with the sustained use of these pouches.
Even though nicotine pouches do not involve tobacco combustion and the associated exposure to harmful smoke and carcinogens, they still contain nicotine. Nicotine can lead to a range of health risks:

Nicotine can be as addictive as any other substance of abuse. But the good news is that it is possible to quit using pouches entirely with the right mindset and strategies. Here are quitting strategies to help you stop using:
The allure of a smoke-free, odorless nicotine delivery method may be appealing, but you should know that nicotine pouches do not eliminate the underlying addiction to nicotine. Quitting nicotine altogether remains the most effective way to improve overall health and well-being. If you're seeking assistance overcoming nicotine addiction, it is best to consult healthcare professionals who can guide and support you in developing a comprehensive cessation plan.
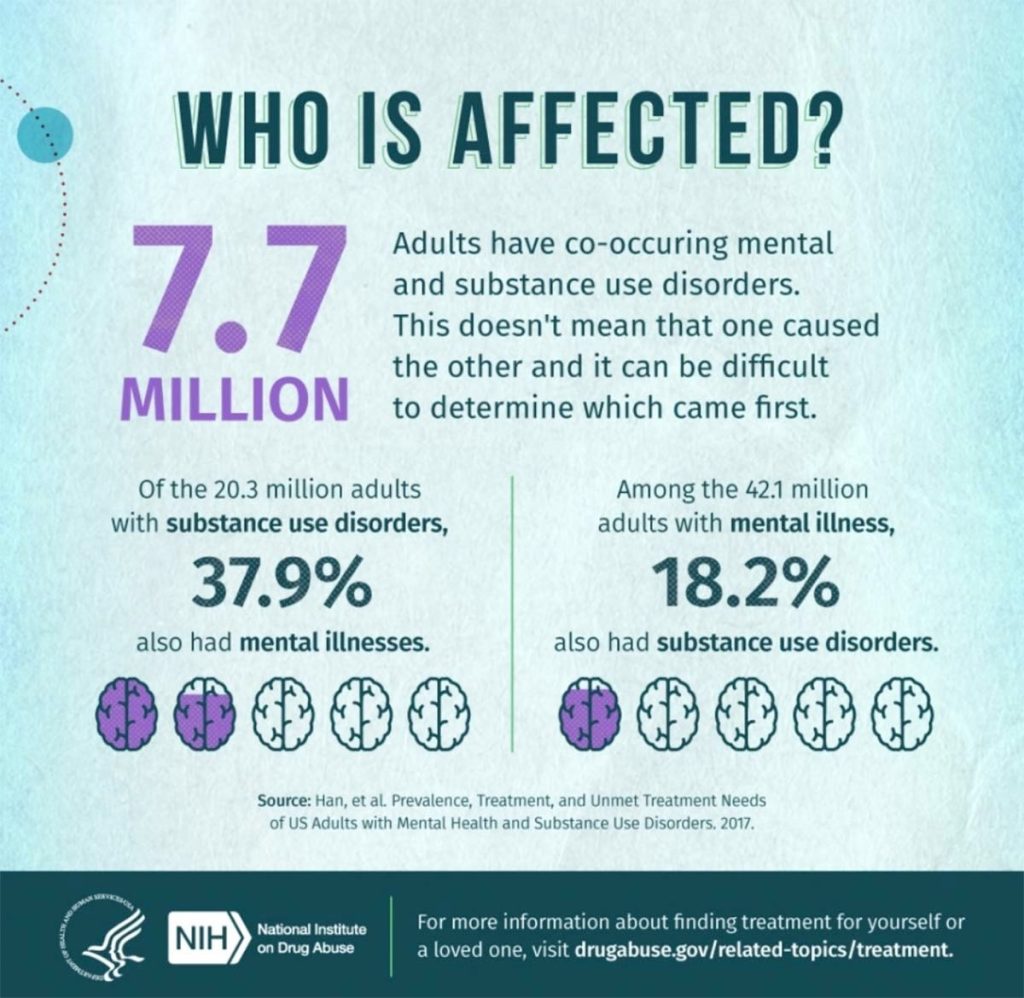
Mental health and addiction issues often go hand in hand, and many people suffer from both. When you have a mental health disorder and substance use disorder at the same time, it is referred to as co-occurring disorders. Co-occurring conditions can be very difficult to manage, as each disorder often significantly impacts the other.
The Substance Abuse and Mental Health Service Administration estimates that about 9.2 million adults in the United States have a co-occurring disorder. Yet, only 7% of those individuals receive treatment for both issues. A whopping 60% of individuals with co-occurring disorders do not receive treatment for either issue. This is a growing concern when it comes to overall public health.
Co-occurring disorders, also known as dual diagnosis or comorbidity, refer to the simultaneous presence of a mental health disorder and a substance use disorder in an individual. This means that an individual may struggle with drug addiction and an underlying mental health condition such as bipolar disorder, depression, anxiety, PTSD, trauma, etc.

Research has shown that people with mental health disorders are more likely to develop a substance use disorder, and people with substance use disorders are more likely to develop a mental health disorder. In fact, roughly about 50% of people with severe mental illnesses are affected by substance abuse and vice versa. This is because individuals may turn to substances as a form of self-medication to cope with their mental health disorder symptoms. Substance use may also worsen existing mental health symptoms or lead to new mental health problems.
Self-medication is one of the main issues surrounding co-occurring disorders. People self-medicate to attempt to numb or cope with the symptoms of their mental health disorder, such as feelings of sadness or worthlessness. However, this is a risk factor for substance abuse and addiction.
Self-medication can also mask the underlying mental health issue, making it difficult for individuals to access the appropriate mental health services. This further perpetuates the cycle of substance abuse, making it even harder for individuals to break free from addiction.

The signs and symptoms of a co-occurring disorder vary depending on the abused substance and mental condition. For example, marijuana abuse and depression could look very different from the signs of alcohol abuse and schizophrenia.
That said, here are some questions you can ask yourself to help determine if you or a loved one may be struggling with comorbidity:
If you answered yes to any of these questions, you may have a dual diagnosis and should consider seeking professional help.
Co-occurring disorders can be challenging to diagnose and treat because the symptoms of the mental health disorder and the addiction tend to overlap. This makes it difficult to determine which condition is causing which symptoms. In some cases, the symptoms might vary in severity, making a patient receive treatment for one disorder while the other disorder remains untreated. People may also be less likely to seek help if they struggle simultaneously with both issues.
But the good thing is that many treatment facilities and professionals (like psychiatrists, psychologists, and therapists) specialize in treating comorbid conditions. These healthcare professionals are experienced in diagnosing and treating substance use and mental health disorders. They will perform a comprehensive assessment that includes physical exams, psychological evaluations, mental health screenings, and substance use assessments to determine the primary and contributing conditions.
Once a dual diagnosis is established, the healthcare provider will create a treatment plan that integrates both mental health and substance abuse treatment co-currently. Addressing these comorbid disorders at the same time ensures the best outcome.

With integrated treatment plans, the same practitioner offers both substance and mental health interventions in an integrated manner. The goal is to treat the person as a ‘whole,’ not just two separate issues. This treatment addresses the underlying causes of addiction, such as depression and anxiety, while providing strategies to help deal with cravings and overcome the physical aspects of addiction.
Integrated treatment often involves specialized therapies such as cognitive behavioral therapy (CBT), dialectical behavior therapy (DBT), motivational therapy, and trauma-informed psychotherapy. Each type of therapy helps address the underlying issues contributing to addiction while promoting healthy coping skills and emotional regulation. These therapies can be offered in individual or group settings.
According to SAMHSA, co-occurring disorders are treated in a stage-wise fashion with different services provided at different stages: engagement, persuasion, active treatment, and relapse prevention. At each stage, a team of professionals provides services that address mental health and substance use disorder.
After treatment, the patient is encouraged to attend support groups, such as Narcotics Anonymous (NA) and Alcoholics Anonymous (AA), to maintain sobriety. Additionally, they are encouraged to use the skills and techniques they learned in therapy, such as mindfulness and stress management, to help them cope with triggers and handle cravings.
Co-occurring disorders are complex conditions that require integrated and comprehensive health services. With the right combination of therapies, medications, and peer support, individuals can recover from mental health disorders and addiction.
People try drugs or alcohol for a variety of reasons, ranging from curiosity or boredom to social pressure or mental health issues. For some people, trying drugs or alcohol is a one-time event that doesn't lead to further use. For others, though, drug or alcohol use can become a substance use disorder, defined as a chronic and relapsing brain disease that is characterized by compulsive drug seeking and use despite harmful consequences.
But what drives people to try drugs and alcohol in the first place? There are several reasons, but some are more common than others.
Peer pressure is one of the leading causes of drug use among young people. Whether it takes the form of subtle suggestions or outright coercion, peer pressure from family and friends can exert a powerful influence over our decisions and behaviors.

Teens are especially susceptible to this type of social pressure, and many will start using drugs at an early age to fit in or feel accepted by their friends. Many young people will try out drugs or alcohol without fully understanding the risks involved.
Mental health issues like anxiety disorders, schizophrenia, eating disorders, bipolar disorders, and depression, can also lead people to start using drugs or alcohol. Numerous studies have listed mental health issues as one of the main drivers of substance use disorders, and vice versa.
Many people with mental health disorders self-medicate in an attempt to numb the pain or ease the symptoms like excessive fear, worry, mood changes, or even suicidal ideation. Others may use drugs or alcohol as a way to cope with difficult life experiences. This can lead to a spiral of drug addiction and mental health problems that is very difficult to break free from.
Trauma, especially early childhood trauma, is a major risk factor for developing substance abuse problems later in life. Traumatic experiences like abuse, neglect, witnessing violence, or losing a loved one can have a profound effect on one's mental and emotional health.
For many people, childhood trauma can be long-lasting and far-reaching, and it's often difficult to overcome the damage done in childhood. They may struggle with mental health issues like Post Traumatic Stress Disorder, anxiety, and depression, and turn to may use substances to try to cope with these problems.
Boredom is another common reason people first try drugs or alcohol. Teens and young adults often have a lot of free time and can be easily bored. They may start using drugs or alcohol to pass the time or to make their lives more exciting. This can lead to addiction, as people continue to use drugs or alcohol to escape the boredom of their everyday lives.

Many young adults first try drugs or alcohol out of curiosity. They may have seen their friends using these substances and want to try them for themselves. Others may be curious about the effects of drugs or alcohol and want to experience them firsthand. It's estimated that over 52% of all high school students try illicit drugs, while over 70% drink alcohol by the time they graduate.
Popular culture often glamorizes drug use, and this can influence young people to start using drugs or alcohol. TV shows, movies, music, and video games often depict drug use in a positive light, and this can make it seem like a harmless or even exciting activity. Constant exposure like this normalizes drug use in entertainment culture. As a result, teens assume using illegal, and prescription drugs is a normal lifestyle.
Many teenagers first start using drugs or alcohol as a way to rebel against their parents or authority figures. They may see drug use as a way to defy the rules and take risks. For example, they may smoke cigarettes to show their independence or hallucinogens to escape to a world they deem more idealistic.
Many people start using drugs or alcohol without knowing much about them. They may believe myths and misconceptions about these substances, which can lead them to underestimate the risks involved. For example, teens might be led to believe that marijuana is medicinal and carries a host of benefits. So, they may be more inclined to start using it without understanding the risks.
People who lack confidence or have low self-esteem are also more likely to start using drugs or alcohol. They may use these substances as a way to boost their confidence or make them feel better about themselves. For example, someone who feels shy in social situations may start drinking alcohol to loosen up and feel more confident.

The above are some of the main reasons people start using drugs or alcohol. It's important to note that not everyone who tries these substances will become addicted. However, drug and alcohol use can lead to addiction, and it’s often hard to break free from this cycle of abuse.
As a parent or guardian, there are a few things you can do to help protect your loved one from addiction:
If you suspect your child is using drugs or alcohol, don't hesitate to reach out for help. There are many physical and mental health care resources available to families struggling with addiction. Early intervention is essential to helping your child get on the path to recovery.
MDMA, also known as ecstasy or Molly, is a synthetic drug that can produce feelings of increased energy, euphoria, and pleasure. It is often used recreationally, at clubs or parties. However, some may be curious whether it is possible to become addicted to ecstasy, or MDMA. The short answer is yes, it is possible to develop a dependence on MDMA. However, addiction is more likely to occur when the drug is used frequently or in high doses. Besides addiction, high doses of MDMA can cause hyperthermia, dehydration, and heart failure. It can also aggravate pre-existing mental health conditions such as anxiety and depression.
MDMA, or 3,4-methylenedioxymethamphetamine, is a psychoactive drug with both stimulant and hallucinogenic properties. It is classified as a Schedule I Controlled Substance in the United States, meaning that it has a high potential for abuse and is not currently accepted for medical use.
When people refer to either Molly or ecstasy, they're referring to the same chemical: MDMA. MDMA by itself is a white or off-white crystal or powder. Molly is the street name for pure MDMA, while ecstasy refers to MDMA that has been cut with other substances. Ecstasy and Molly can come in pill form, but Molly is most often sold in powder form.
MDMA, in its pure form, is difficult to come by. Dealers often cut MDMA with other drugs like amphetamines, cocaine, ketamine, caffeine, synthetic cathinones, LSD, rat poison, and heroin to strengthen its effects and increase profit margins. Cutting MDMA with these illicit drugs increases the risk of adverse effects and overdose deaths.

MDMA is primarily used as a party drug due to its ability to induce euphoria, increased emotionality, and increased sensation. So, it's mostly found in house parties, raves, and music festivals. While MDMA is considered a harmless party drug, it can be very dangerous if not used responsibly. According to statistics, the number of emergency room visits increased by 1,200% since ecstasy became popular at all night-raves.
MDMA increases neurotransmitters serotonin, dopamine, and norepinephrine levels in the brain. These brain chemicals are associated with mood, energy, and alertness. They also cause users to become more stimulated and awake. However, MDMA can also have negative side effects, such as:
When combined with a hot environment, physical activity, and other drugs, MDMA can lead to unpredictable and serious physical complications. The drug causes hyperthermia, significant dehydration, or cardiovascular collapse, leading to kidney, liver, or heart failure and even death.
The effects of ecstasy can kick in within 20 minutes and typically last for 3-5 hours but can persist for up to 8 hours. This variation can be due to factors like body weight, the amount used, gender, mode of administration, etc.
One of the most serious risks of MDMA use is addiction. While the exact mechanisms are not fully understood, it is clear that MDMA can cause changes in brain chemistry that lead to compulsive drug-seeking behavior and an inability to control use.
Although MDMA has been shown to be addictive in animal studies, the degree of self-administration is relatively low compared to other drugs such as cocaine. This suggests that while MDMA may have some potential for addiction, it is not as strong as other substances.

Data from animals and humans suggest that regular use of MDMA leads to adaptations in the serotonin and dopamine systems linked to substance use disorder and related behaviors, like increased impulsivity.
Some studies have tried to analyze MDMA dependency or addiction among people with a history of use in the general population. The results of these studies have varied widely, probably due to different population samples and different types of measures used. However, some people who use MDMA do report symptoms of addiction, including:
MDMA is a stimulant drug with properties similar to other drugs in its class, like cocaine. While research is inconclusive on whether MDMA is addictive, heavy or regular drug use may lead to addiction. Additionally, MDMA is often mixed with other stimulants, increasing the risk of addiction.
The mix of drugs sold as ecstasy may alter how people who take it react to it, making it difficult to predict if someone may develop an addiction. However, what is clear is that regular or heavy drug use can lead to addiction. Therefore, it is important for those who use MDMA to be aware of the risks associated with the drug.
Some people might not consider MDMA an addicting drug. Even so, there are still dangers associated with its use.
When people take MDMA, they risk because the drug is unregulated, and its purity can't be guaranteed. One of the biggest dangers is that it is often cut with other substances, which can be dangerous or even deadly.
For example, one of the most common adulterants is methamphetamine, which can lead to increased blood pressure and heart rate, as well as anxiety and paranoia.

Sometimes, these effects can be so severe that they result in hospitalization or even death. In addition, MDMA is often cut with other substances that may not be immediately harmful but can still cause long-term damage, such as liver damage.
MDMA can also cause tolerance. This means that users need to take increasingly larger doses to achieve the same effects. Tolerance can lead to physical dependence and addiction. It can also increase the risk of overdose and other health problems.
Increasing the dose to achieve the same effect may also lead someone to use other drugs, which can lead to addiction - and potential overdose. Statistics show that 92% of those who start using ecstasy resolve to using amphetamines, marijuana, heroin, and cocaine later on.
Using other drugs to cope with the mental and physical pain that results from ecstasy can quickly spiral out of control, leading to addiction to other drugs and potentially serious health consequences.
If you or someone you know is struggling with an addiction to MDMA or any other form of drug abuse, please seek professional help. Treatment options are available, and there is always hope for recovery.